Perspectives with Max Wicha
interview by Nicole Fawcett
We might for the first time really be thinking of cures of cancer
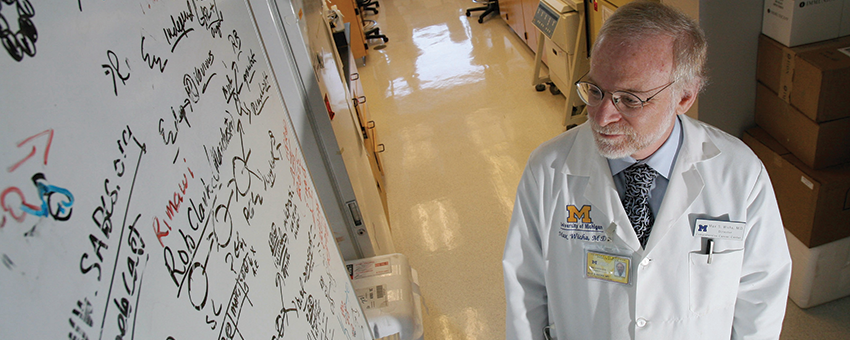
Photo credit: New York Times
When Max Wicha, M.D., was starting his career, oncology did not come highly recommended.
"When I first got into this field about 40 years ago, I went for advice to someone who was very senior in medicine. I said I want to go into cancer research and become an oncologist. They looked at me and said, 'Why would you want to waste your life on that? We're not going to make progress against cancer. It's the least scientific of any discipline. Go into some other field where you can really use science,'" Wicha recalled.
"Of course, that turned out to be completely wrong."
In fact, Wicha, the Madeline and Sidney Forbes Professor of Oncology and founding director of the Rogel Cancer Center, jumped into the discipline just as it was taking off.
On the heels of the National Cancer Act's 50th anniversary, Wicha reflects on the evolution of the field.
When you were getting started, were you surprised by your mentor's criticism of the field?
What they said in a sense was true. Forty years ago, there was a tremendous disconnect between research to understand the biology of cancer and the clinical practice of oncology. The clinical care had very little to do with the science that was brewing in the laboratory.
Initially, when chemotherapy was developed, medical oncologists thought if we find the right combination of chemotherapy, we can cure most patients with cancer. That turned out to be naïve, and there was a lot of discouragement among clinicians when their clinical trials didn’t improve outcomes.
At the same time, basic scientists were coming up with dramatic results in the laboratory, with the first discoveries of oncogenes and tumor suppressor genes.
The basic scientists were saying, 'Look, we're starting to understand what cancer is.' But if you went to the clinic, you didn’t see any impact. That was the dichotomy of the field.
How did the National Cancer Act and the beginning of cancer centers start to change this?
To make a fundamental impact, we knew we had to take the basic research and figure out how it leads to improvements for patients — not just make discoveries in the laboratory.
Cancer centers became a lot of the engine for cancer research and cancer discovery, which propelled us into the dramatic impact we see now. It’s because of this marriage of basic research, clinical research and what we now call translational research.
When you were tasked with creating a cancer center at the University of Michigan, how did this landscape influence your approach?
The challenge was how to get these groups to merge and talk to each other. On the clinical side, we had people in each discipline treating patients in different ways. Not only did they not talk to the basic laboratory scientists, but even more challenging, they didn't talk to each other.
In my own field of breast cancer, a woman then would have to visit multiple specialists, sometimes getting contradictory opinions. It could take more than a month. Patients would say, 'Why don't you put your heads together.' Of course, that was the right advice.
When we started organizing our cancer center, we decided to experiment with a multidisciplinary breast clinic. We organized either the first or second multidisciplinary clinic in the country. It was a success right from the beginning. Now of course everyone does it.
Then when we started organizing a cancer center, I thought the way to do this was around multidisciplinary programs for each type of cancer. It allowed us for the first time to bring together active teams of people from different disciplines who work on a particular cancer.
It enabled us to start introducing basic scientists to clinicians and move to a more scientific approach to treat patients.
Where are we now in the progress against cancer?

Photo credit: Leisa Thompson
It's completely flipped around. Right now, cancer is the most scientific discipline. It's the best example of basic research discoveries changing clinical care.
Melanoma is a good example. First, we developed molecular targeted therapies based on specific mutations in the tumor. But even more successful has been the use of immune stimulators. Here's a disease that was completely fatal. Now, about 60% of patients see a very significant benefit from immunotherapy. Even more exciting, for aa percentage of patients, the melanoma isn't coming back. We might for the first time really be thinking of cures of cancer.
In my field of breast cancer, we’ve developed so many different treatments that often we can turn metastatic cancers into chronic diseases. I have patients who have had metastatic breast cancer for over 20 years.
The trick now is to understand what’s different about the exceptional responders and get more patients into that realm. And the real challenge is going to be how to apply this to tumors where we haven't made much progress, like pancreas cancer and brain tumors.
I will almost guarantee you that progress in those areas won't be by accident but by studying the basic biology of those cancers and then applying new ideas based on that.
Are you glad you decided to go into oncology after all?
Personally, it's been such a privilege, and I've been so fortunate to have been in oncology during this phase when it went from a primitive discipline to being a scientific discipline making huge advances.
4 Biggest Cancer Research Breakthroughs
Major recent breakthroughs in cancer research are leading to cures and turning metastatic cancer into more of a chronic, managed disease. These are four areas of research Max Wicha, M.D., says are having the biggest impact:
Immunotherapy Wicha called this 'the biggest breakthrough in cancer research over the last decade." Ongoing work will uncover how to make immunotherapy effective for more patients. |
Targeted therapies These treatments have led to huge progress in breast cancer, melanoma, lung cancer and others by targeting specific genetic alterations within tumors. |
Epigenetics Tumors can change from one type of cell to another, leading researchers to explore the idea of manipulating the epigenome to find new ways to attack cancer. |
Cancer metabolism Different cancers have common metabolic endpoints. Can targeting these commonalities make it harder for the tumor to develop resistance, since all the mutations funnel downstream to them? |
Continue reading the online version of Illuminate Winter 2022 issue:
- The Cancer Microbiome
- Found in Translation
- Emphasizing Equity
- Bringing Harmony to Advanced Breast Cancer Care
- Let's Talk About How We Talk About Race
- Feedback Loops
- Probing a Cancer Paradox
Print/download the Winter, 2022 issue of ILLUMINATE.
Get research news in your inbox!
Our Illuminate e-newsletter showcases the important and unique research underway at the Rogel Cancer Center.
Follow this link and sign-up today!
