The Cancer Microbiome
contributed by Sarah Kearns, Ph.D., and Ian Demsky
Scientists are just starting to appreciate the many ways microbes influence the initiation, progression and treatment of cancer. Here’s what Rogel researchers are learning.
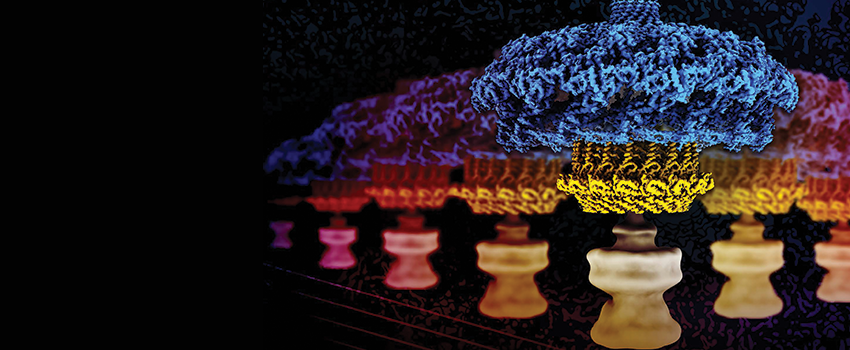
Photo courtesy of the Ohi laboratory
In 2016, a group of scientists publishing in PLOS Biology estimated that our bodies contain not the commonly accepted 10 human cells for every one microorganism, but something closer to a 1-to-1 ratio — with these tiny counterparts collectively weighing 4 or 5 pounds.
This "other half" of us plays a vital role in human health, with symbiont communities thriving on our skin, and in our mouths, noses, lungs, digestive tracts and a host of other organs. And researchers are just starting to probe the multiplicity of roles these organisms can play in the initiation, progression and treatment of cancer.
This new appreciation has led to growing efforts at the University of Michigan Health Rogel Cancer Center, and elsewhere around the globe, to harness the power of the microbiome to prevent cancer and improve therapies.
"H. pylori don’t want to give anyone stomach cancer," says Melanie Ohi, Ph.D., a professor of cell and developmental biology. "They're just trying to create a niche to live in."
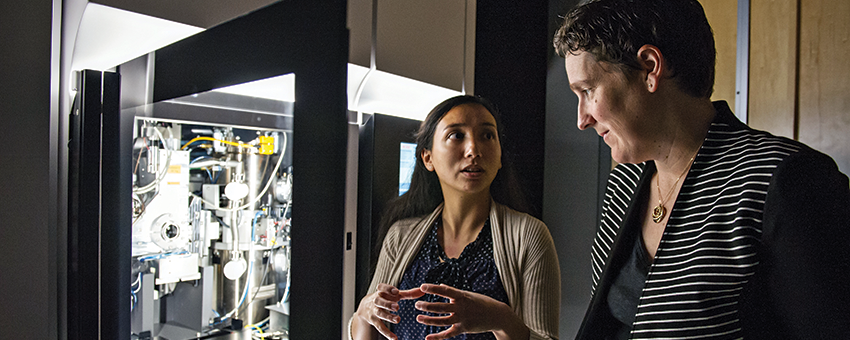
Over the last several years, Ohi’s lab at the U-M Life Sciences Institute has used cryo-electron microscopy to capture, in increasing detail, near atomic-level 3D snapshots of the molecular machinery that Helicobacter pylori uses to infect host cells, triggering the chronic inflammation that can lead to the development of gastric cancer.
While roughly half the human population has been colonized by the bacterium, most people never experience any ill effects. Still, H. pylori infection is the strongest known risk factor for stomach cancer, which is the fourth-most deadly type of cancer worldwide, according to the World Health Organization.
Ohi’s team and their collaborators published the best views to date of the bacterium’s secretion system in eLife, revealing two species-specific components, and greatly improved resolution of its spokes and outer ring.
Ohi likens this structural biology approach to developing a schematic of the inside of a lock to figure out the exact size and shape of the key you need.
"By understanding how these molecular machines move, how each part of the secretion system functions, our goal is to find new ways to target the processes that cause disease," she says.
Forests and trees
One of the challenges for studying the relationships between our microbiomes and cancer is that they’re both varied, dynamic and complex systems in their own rights.
Plus, there’s no one-size-fits-all microbiome. Individuals can have healthy, stable populations of gut bacteria made up of different species due to factors including inheritance, geographic location and diet.
"You can have many different ecosystems that could be considered to be healthy. A jungle in the Amazon can be just as healthy and productive as a redwood forest," says Vincent B. Young, M.D., Ph.D., a professor of internal medicine and of microbiology and immunology, whose lab studies the microbial ecology of gastrointestinal infections.
Moreover, the complexities of interactions between microbes and hosts are staggering, he notes. Bacteria that have co-evolved with humans can play both detrimental and positive roles in different aspects of health. For example, testing for and treating H. pylori is of clear benefit for lowering the incidence of stomach cancer. At the same time, infection with the bacterium has also been associated with reduced risk for asthma, inflammatory bowel disease and acid reflux, which is in turn a risk factor for esophageal cancer.
Accordingly, a multidisciplinary approach is needed — one that brings together expertise in microbial ecology, immunology, cancer cell biology and computational biology, Young and co-authors including cancer center member Thomas Schmidt, Ph.D., argue in a 2020 Trends in Cancer editorial.
"Each cancer is itself an ecosystem in which cancer cells interact with each other and with stromal cells in intricate, dynamic ways," the authors write. "Common factors such as circulating metabolites, systemic immunity, etc. can impact on — and be affected by — the two types of ecosystems simultaneously. The relevant links between microbiomes and cancers may be impossible to reduce to a single component."
These interactions can be both cooperative and competitive, notes Yatrik Shah, Ph.D., a professor of molecular and integrative physiology and of internal medicine.
"A tumor is a very needy accumulation of cells," says Shah, who studies gastrointestinal homeostasis, inflammation and cancer. "It takes up nutrients, many of which the microbiome would rather be using. So, that forces the microbiome to adapt."
As cancer develops, it changes the abundance of particular species of bacteria within its environment, often reducing populations of beneficial bacteria, he says. Then, once the tumor has established itself and altered the microbiome to its liking, the bacteria that are left are likely to be complicit in tumor growth and even promote cancer progression.
"It really remakes its environment to suit its own needs," Shah says.
Patrick Schloss, Ph.D., a professor of microbiology and immunology, has also been studying these dynamic interactions — especially the impact that perturbations of the microbiome can have on human health, including the development of cancer.
One area his group has focused on is oral microbes' contribution to tumor growth in colorectal cancer.
People with colon cancer often have populations of bacteria in their gut that are typically found solely in the mouth — organisms like Fusobacterium nucleatum and species of Porphyromonas.
"Even though healthy individuals are swallowing saliva every day, you won't see these populations in their gut," Schloss says. "So, there's something interesting going on with their relationship to colorectal cancer."
The conditions for tumor initiation in colon cancer depend less on any single factor — individual bad microbial actors, specific bacterial virulence factors, disruption of signaling pathways, or promotion of inflammation — than on all of these components working in concert, he says.
And then added into this mix are the uniquely stubborn properties of oral microbe colonies when they glom together in sticky matrices called biofilms.
"Big picture: This means that as scientists are designing new studies, creating screening tests based on the microbiome, or developing new therapeutic interventions, we really need to be taking the entire microbial community in and around tumors into consideration rather than just zeroing in on individual pathogens," says Schloss, whose group is also interested in the role of virus communities — or the virome — in the development of colorectal cancer, largely through their modulation of bacterial communities.
Different bacteria, different levels of cancer
Identifying specific members of the gut microbiome that contribute to the development of cancer is challenging because of the natural variation in microbial communities between individuals, says Grace Chen, M.D., Ph.D., an associate professor of hematology/oncology.
Scientists have found significant differences between the bacteria found in patients with colorectal cancer and those without, but it has been difficult to reach strong conclusions about causation because of the natural dissimilarities between one person and another and the lack of longitudinal studies, she says.
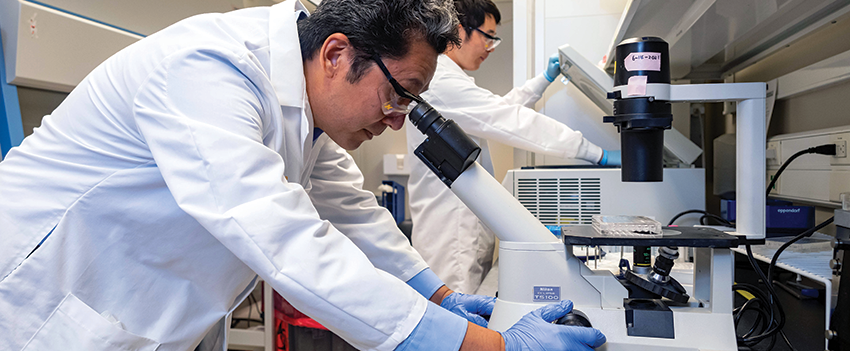
To overcome this hurdle, Chen uses specialized mouse models ‐ either developed to lack any microbial communities or colonized by only specific bacteria — to study how the host immune system and the gut microbiome affect intestinal inflammation and the development of cancer.

"In controlled mouse studies, we were able to demonstrate specific changes to the microbiome during the development of inflammation and tumors, and that these changes directly cause disease," adds Chen, who frequently collaborates with Schloss.
Several recent studies from her lab showcase just how powerful these changes can be.
For example, different microbiomes can be associated with different levels of immune cell stimulation, specifically CD8+ T cells, Chen’s group found. And while these T cells normally help protect the body against cancer, overstimulating them can potentially promote inflammation and exhaust the T cells — which can actually increase susceptibility to cancer, according to findings they published in Cell Reports.
"There has also been a lot of excitement about the role bacteria may play in improving the effectiveness of immunotherapy by promoting T cell activation," Chen says. "This work suggests it may be a double-edged sword — and that in the context of an unhealthy microbiome, the promotion of T cell exhaustion is something researchers need to watch out for."
In cancer patients, disruption of the healthy gut microbiome has been associated with poorer responses to treatment with immune checkpoint inhibitors, so there has been keen interest in making targeted adjustments to improve outcomes.
Chen’s findings grew out of experiments that showed the powerful influence of the microbiome in the development of cancer when genetics are taken out of the picture.
Starting with two groups of genetically different mice, each with distinct microbiomes, they found that the one group fared better than the other when exposed to the same carcinogen.
Then the team ran another experiment, transplanting the microbiomes from each group of mice into two new, genetically identical colonies of germ-free mice. Again, mice who shared bacteria with the original second colony developed more tumors.
"This showed that the composition of the gut microbiota can directly influence tumor development," Chen says. The team also identified specific bacteria that consistently correlated with more tumors — findings which will need to be further validated.
Chen’s team next conducted experiments to better understand what was driving the increased inflammation and tumor growth. Through immune cell profiling, they found that there were more T cells in the colon tissue of mice with bacteria from the second colony, and many more CD8+ cells.
"It's a little counterintuitive, since T cells and CD8+ cells are usually associated with better outcomes in colorectal cancer patients," Chen says. "We hypothesize that these cells get over-activated in the presence of certain bacteria and then exhausted, leaving them less capable of killing tumor cells.
Bridging bench and bedside
Scientists are just starting to understand the ways good and bad gut microbes adapt as healthy conditions shift toward disease.
A team led by Kathleen Cho, M.D., the Peter A. Ward Professor of Pathology and director of gynecologic pathology at U-M, recently investigated the influence of the microbiome on the development of ovarian cancer and related cancers of the upper genital tract in a mouse model of high-grade serous carcinoma.
Half of the mice in the study were given antibiotics, which changed the composition of the bacteria in their digestive and reproductive tracts. Compared to control mice, the treated mice developed significantly fewer tumors and their cancer was less advanced at the end of the study period, according to findings that the group published in Cancer Research.
"This is a close model of human ovarian cancer, and our findings suggest that the microbiome does influence its pathogenesis," Cho says. "This model system could be used to explore whether manipulating the microbiome could improve ovarian cancer’s generally poor response to immunotherapies."
Meanwhile, Nobuhiko Kamada, Ph.D., an associate professor of internal medicine, has been investigating how intestinal inflammation actually reprograms the metabolic pathways of gut bacteria such as E. coli, allowing them to thrive in changing environments. Over time, chronic inflammation and related immune changes in the gut can promote the development of cancer.
E. coli shifts its metabolism to make use of the amino acid L-serine to maximize its growth potential," says Kamada, whose lab focuses on how the gut microbiome and host immunity influence gastrointestinal health and disease.
Withholding amino acids from the diet, particularly L-serine, blunted inflammation-induced E. coli growth in mouse models — and did so without disrupting the host immune response, his group recently reported in Nature Microbiology.
"Our findings suggest dietary interventions to influence nutrient availability could help against diseases driven by disruptions of the healthy gut microbiome — like inflammatory bowel disease, which is a major risk factor for cancer," he says. "They also point toward L-serine utilization pathways as potential therapeutic targets to inhibit the growth of certain pathogenic bacteria without harming beneficial bacteria."
Kamada and Chen were also collaborators on an effort led by James Moon, Ph.D., the John G. Searle Associate Professor of Pharmaceutical Sciences at the U-M College of Pharmacy, to develop a dietary fiber gel that holds promise for improving the potency of immunotherapies against cancer.
"It's amazing to think that something as simple and safe as eating more of a dietary fiber like inulin could make such a big difference,” Moon says.
Inulin, a fiber found in chicory root, Jerusalem artichoke and other plants, is a prebiotic that provides a rich source of nutrients to beneficial microbes, helping them to proliferate.
"Importantly, the benefits go beyond colon cancer," he notes. "The changes in the gut microbiome stimulate cells, which circulate throughout the body amplifying the activity of immunotherapy treatment."
The inulin gel improved immune checkpoint inhibitor therapy in mice with skin cancer as well as those with colon cancer, the group reported in Nature Biomedical Engineering.
Additionally, inulin was approved by the Food and Drug Administration in 2018, which will shorten the hurdles of moving the findings in mouse models into human clinical studies, Moon adds.
"We and others have shown that the gut microbiome has a crucial role in our immune responses," notes study first author Kai Han, Ph.D., a postdoctoral fellow in Moon’s lab. “Close to 70% of lymph nodes in our bodies are located in the gastrointestinal tract and, therefore, microbes residing in the gastrointestinal tract closely interact with our immune cells. Maintaining a healthy gut microbiome nurtures our immune system so that our immune cells can effectively fight against cancer."
And that’s not the only place Rogel researchers are looking to leverage the microbiome in the clinic. A group of investigators from diverse fields and schools recently received an $11.2 million grant from the National Heart, Lung and Blood Institute for a multi-pronged project aimed at reducing graft-versus-host disease — a common and potentially deadly complication of stem cell transplants used to treat blood cancers and other diseases.
Together, the work will explore the importance of the microbiome, and key metabolites produced by microbes in mitigating the severity of GVHD and improving outcomes. The effort includes both studies in mice and also a proof-of-concept clinical trial looking at the impact of dietary adjustments on patients' microbiome, metabolome and clinical outcomes.
"This project brings together a team who have worked and published together previously," says principal investigator Pavan Reddy, M.D., deputy director of the Rogel Cancer Center and division chief of hematology/oncology. "These collective projects are the results of unifying our preliminary datasets over the past several years. We hope that by working collaboratively we can make a difference for patients receiving hematopoietic cell transplants."
Drugs from Nature's pharmacy

While other scientists work to better understand the complex interactions between bacteria and their human hosts, Rogel Cancer Center member David H. Sherman, Ph.D., looks to tap into the rich biochemistry that has evolved inside microbes to pioneer new anti-cancer drugs and other medicines.
Sherman, the Hans W. Vahlteich Professor of Medicinal Chemistry at the College of Pharmacy, has conducted diving expeditions and trips to remote locations around the globe to collect rare bacteria that might harbor the next big breakthrough.
"Symbiotic microbes have long been thought to be the true sources of many of the natural products that have been isolated from invertebrates in the ocean and on the land — but very little is known about them because it’s extremely difficult to identify them and culture them in the lab," Sherman says.
A few years ago, for example, Sherman’s group pinpointed the true origins of an anti-cancer compound known as ET-743, or trabectedin, which had originally been harvested from a type of sea squirt. By analyzing the genome of this mangrove tunicate along with the microbes that live inside it, the team was able to isolate the genetic blueprint of ET-743’s producer — a bacterium known as Candidatus Endoecteinascidia frumentensis.
"Currently, many of these compounds can only be harvested in small amounts from host animals, which is unsustainable from an economic and environmental perspective," says Sherman, who also holds appointments at the U-M Life Sciences Institute, Medical School and College of Literature, Science, and the Arts. "Our hope is that understanding the genomes of these microorganisms and the chemical reactions that occur inside them will provide new avenues to economical and sustainable production of the medicinal molecules they make.
Continue reading the online version of Illuminate Winter 2022 issue:
- Found in Translation
- Emphasizing Equity
- Perspectives with Max Wicha
- Bringing Harmony to Advanced Breast Cancer Care
- Let's Talk About How We Talk About Race
- Feedback Loops
- Probing a Cancer Paradox
Print/download the Winter, 2022 issue of ILLUMINATE.
Get research news in your inbox!
Our Illuminate e-newsletter showcases the important and unique research underway at the Rogel Cancer Center.
Follow this link and sign-up today!
