Glioblastoma Patient is Beating the Odds
Initially given 16 months to live, doctors at the U-M Rogel Cancer Center helped Kathy Bellmore to beat the odds and to continue to make memories

Photo credit: Bryan McCullough, Michigan Medicine
One day this fall, Kathy Bellmore’s phone rang. It was her eldest son.
He asked if she knew what day it was.
“I thought maybe I missed somebody’s birthday,” she recalls during a recent interview.
But her son was calling to mark a different kind of anniversary.
Sixteen months earlier, Bellmore, a retired St. Johns elementary school teacher from Dewitt, Mich., had been diagnosed with high-grade glioblastoma multiforme, an aggressive brain tumor with few good treatment options.
The hospital where she was initially seen told her the tumor was inoperable and estimated she would likely live only another 12 to 16 months.
Sometimes called “The Terminator” due to its fast and deadly nature, glioblastoma has a median survival time of nine months without treatment and an additional seven months with standard therapies, researchers have noted.
Following treatment at the University of Michigan Rogel Cancer Center however, Bellmore hit that 16-month mark in October -- and is still going strong.
“Words can’t express how thankful I am for all of the support, kindness and knowledge you have surrounded me with,” she wrote to her neuro-oncologist, Yoshie Umemura, M.D., on that 16-month anniversary, also adding her gratitude to the other doctors on her care team, her nurses and all of the hospital staff.
The time since her diagnosis has been filled with love, family, travel and special memories, Bellmore says.
“We are just so blessed,” she says.
From patient to research participant
Bellmore started to realize things were amiss in the spring of 2018.
“I was at the mall and I went to put on the brake and all of a sudden my car accelerated,” Bellmore says. “And I thought, ‘That stupid car.’”
There were a few other little signs like that here and there until one day Bellmore’s foot started fluttering and wouldn’t stop. They called for an ambulance and went to a local hospital.
“I was crying. I said to the nurse, ‘You can’t send me home. I know something is wrong. You just have to find out.’ I think and pray about her all the time because she brought in a neurologist, who ordered an MRI of my brain.”
That scan and a subsequent biopsy revealed a worst-case scenario: a malignant tumor.
After initially being told that surgery wasn’t an option, Bellmore sought a second opinion at U-M and received more hopeful news.
“When Dr. Umemura called us that Friday after the U-M tumor board met to discuss my case, we were in Bellaire picking out my tombstone,” Bellmore says. “She said they would take my case and could perform surgery.”
In August 2018, over the course of a seven-hour operation, neurosurgeon Oren Sagher, M.D. was able to remove most of the tumor.
“There’s a little piece the size of a fingertip they weren’t able to remove because of where it was,” Bellmore says.
Bellmore learned she was also eligible to participate in a clinical research study that added an experimental gene therapy to the standard treatment with radiation and chemotherapy.
The study, which is active but not currently enrolling patients, aims to investigate the safety of a new approach to treating glioblastoma. Participants had two modified adenoviruses injected into their tumors. These “virus vectors” had been altered to deliver therapy rather than cause disease.
Given the grim prognosis for patients with glioblastoma, Bellmore decided to volunteer.
“We have an amazing, loving family, including three children, two daughters-in-law and six grandchildren,” she says. “You don’t want to leave them. But at that time I truly felt like if this is my time, I could go, because I’ve lived a good life.
“You always have to look up and not down,” Bellmore adds. “My name is Kathleen Grace and I’ve always felt that God surrounds me in grace.”
Making Memories
The last year and a half haven’t been easy for Bellmore and her family. Last fall, there were six weeks of near daily radiation treatments and chemotherapy pills. This fall, a tumble led to a broken arm that has slowed her down a little further.
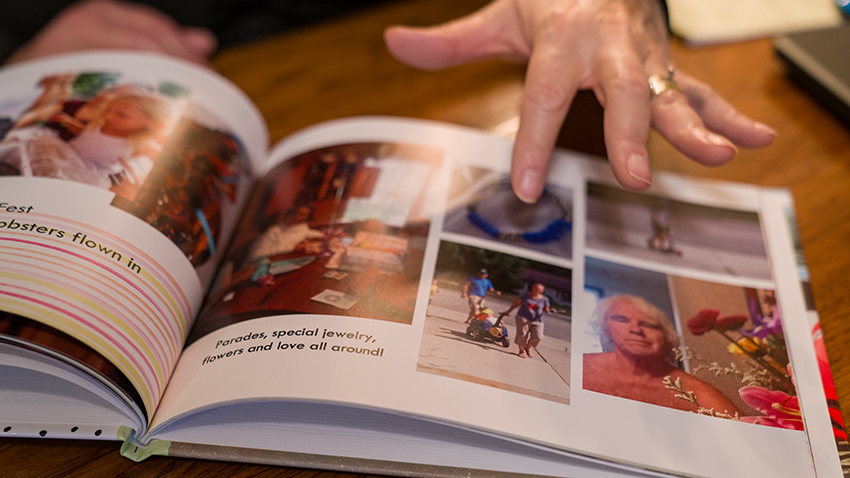
But there’s also been a lot of wonderful family time and memory-making, too, say Bellmore and her husband Paul while showing off photo books at their kitchen table.
One of their trips was to Marquette, home of Northern Michigan University, where the couple met and fell in love.
“We’re Wildcats,” she says. “We went back to all of our favorite places, went walking by the Dead River Falls. We saw Cheech and Chong there back in 1970-whatever.”
Paul adds, “We went back to what we used to think was the best restaurant ever -- The Villa Capri.”
It’s easy to see how in love they still are. At one point in the interview, Kathy slips and says, “when we were diagnosed” instead of “when I was diagnosed.”
“I have my family and my friends and my prayer group, but my biggest strength is sitting right here next to me,” Kathy says of Paul. “How many people have that in their lives? You just don’t want to leave each other.”

Photo credit: Bryan McCullough, Michigan Medicine
“We’re a team,” he agrees.
The couple is preparing to celebrate their 46th wedding anniversary on Dec. 29.
Looking toward the future
Today, Bellmore says she’s doing well. Doctors are continuing to monitor her tumor, which so far isn’t regrowing.
“I truly believe every day is a gift,” she says.
Umemura, Kathy’s neuro-oncologist, adds, “Kathy and her husband, Paul, are a great example of positively coping with the knowns and unknowns of a difficult diagnosis. It’s inspiring to see how they prioritize things that are in their control, and stay optimistic while still being realistic. They inspire me to pay more attention to the things that are really important in my own life -- if they can do it, I can do it, too.”
Asked what advice she has for other patients in a similar situation, Bellmore stresses the importance of having strong support systems, which for her includes family, friends and faith.
She also says that patients shouldn’t be afraid to advocate for themselves.
“Get a second opinion,” she says. “You want to trust all doctors in all places, but it can’t hurt to get a second opinion.”
