Why Every Pancreatic Cancer Patient Should Consider Genetic Testing
An expert panel finds an inherited risk in 1 in 10 pancreatic cancer cases, leading to new recommendations advising all patients to consider genetic screening.
Genetics may play a larger role in pancreatic cancer than previously thought, an expert panel has found.
It’s led to the American Society of Clinical Oncology recommending that genetic testing be offered to anyone diagnosed with pancreatic cancer.
The goal: to help identify family members who might be at greater risk.
“It now appears that as many as 1 in 10 patients diagnosed with pancreatic cancer carry a genetic alteration associated with an increased risk of pancreatic or other cancer types,” says Elena Stoffel, M.D., MPH, a gastroenterologist and director of the Cancer Genetics Clinic at the University of Michigan Rogel Cancer Center.
“If family members learn they may be at risk for pancreatic or other cancer types, they have more opportunities to take action.”
Stoffel, who was part of the expert panel that developed the new recommendation, explains what it means for patients and families:
Genetic testing for pancreatic cancer
What is the new recommendation?
Stoffel: It calls for all patients diagnosed with pancreatic cancer to receive genetic counseling related to their risk for inherited syndromes associated with an increased risk for pancreatic cancer.
That assessment begins with a comprehensive review of family history of cancer.
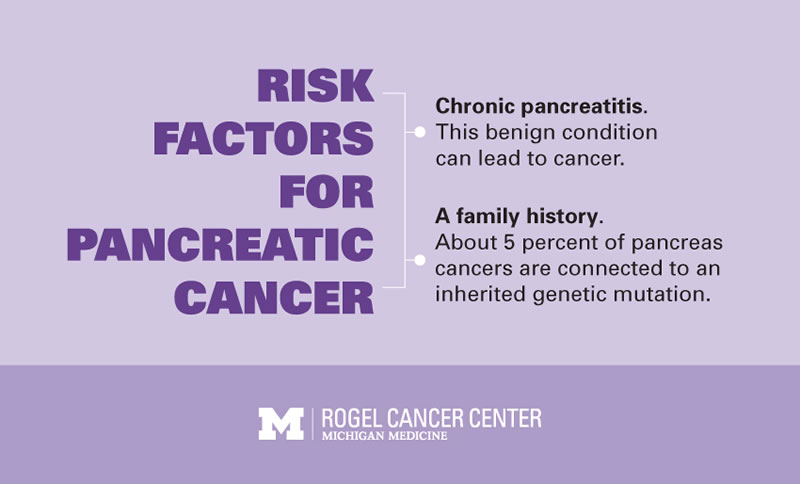
Individuals with two first-degree relatives with pancreatic cancer meet the criteria for familial pancreatic cancer. Individuals (with or without cancer) from these families, individuals with three or more diagnoses of pancreatic cancer on the same side of the family and individuals who meet the criteria for other genetic syndromes associated with pancreatic cancer all are at elevated risk for developing pancreatic cancer and are also candidates for genetic testing.
Even if only one family member had pancreatic cancer, some cancer diagnoses in other family members — such as early age breast cancer, ovarian cancer, colorectal cancer or gynecological cancers — may also meet the criteria for genetic testing.
What led to this new recommendation?
Stoffel: Several recently published studies have shown that the percentage of pancreatic cancer patients with a genetic predisposition to cancer is higher than expected.
I was part of a panel of specialists convened by ASCO to review about 20 years of research, as well as our own case files, and condense everything we know so far about the link between genetics and pancreatic cancer.
We concluded that, while 90 percent of patients have no detectable genetic alterations associated with cancer risk, genetic testing finds an inherited factor in 10 percent — information that could help doctors tailor cancer screening to detect pancreatic (and other) cancers earlier, when they are more treatable.
What do you hope this recommendation achieves?
Stoffel: If patients with pancreatic cancer undergo genetic testing and it shows that an inherited genetic alteration increased their cancer risk, then their close relatives may share that genetic predisposition and that elevated risk of developing pancreatic cancer.
Because some of the genetic alterations identified in pancreatic cancer patients are associated with risk for other cancers (such as breast cancer) for which screening does have a proven benefit, genetic test results from patients with pancreatic cancer could have a big impact on the health care decisions of their family members.
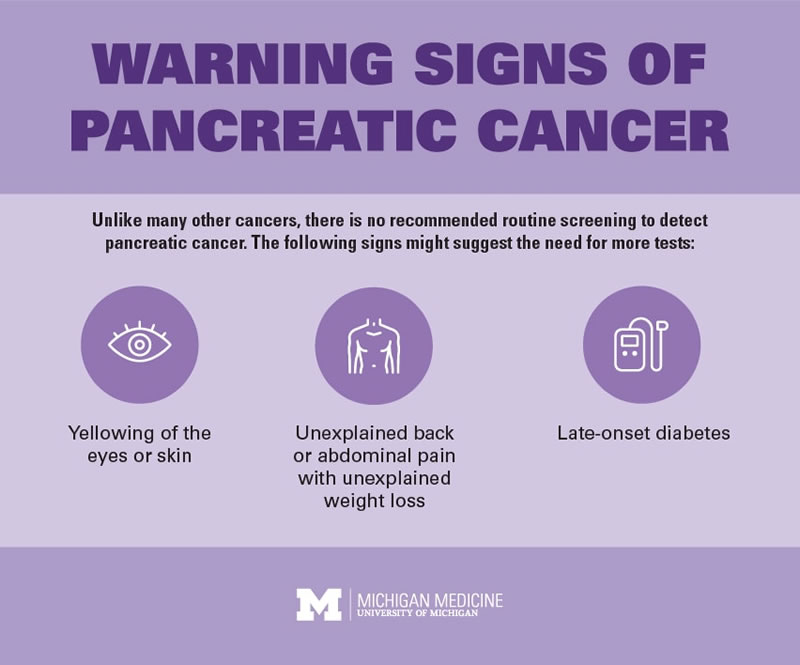
Currently, there is no screening test proven to reduce mortality from pancreatic cancer. By the time a patient experiences symptoms, the pancreatic cancer is usually too advanced to treat.
But many times, we find early stage pancreatic cancer while screening for something else. When found early, pancreatic cancer is more likely curable.
As clinicians, all of us on the ASCO panel have had anecdotal experience finding cancers early based on screening. The results can be lifesaving.
What kind of recommendation is this?
Stoffel: ASCO issued what is called a provisional clinical opinion, or PCO. A PCO alerts doctors and patients that, although there is not yet enough data to draw a truly evidence-based conclusion, based on the consensus opinion of experts it is anticipated that a clinical recommendation is coming.
It’s worth noting that ASCO does not issue PCOs casually. Their goal is to back up every recommendation with definitive research.
To date, there are only two studies showing benefit for pancreatic cancer screening, but we made the case that that doesn’t mean we shouldn’t be screening individuals at high risk for pancreatic cancer now.
What genes are you looking for?
Stoffel: The PCO contains a list of about a dozen genes for which we recommend screening. Many are familiar culprits — there’s a great deal of overlap among the hereditary cancers associated with alterations in these genes.
For instance, we look for mutations in the DNA repair genes BRCA1, BRCA2 and PALB2. These are known to drive hereditary breast and ovarian cancer but are also linked to pancreatic cancer.
We also look at the genes associated with Lynch syndrome, a hereditary condition associated with high risks for colon, endometrial and other cancer types, including pancreatic cancer.
Mutations in other genes, including p16 or CDKN2A, are also linked to pancreatic cancer risk.
What steps should family members take based on genetic test results?
Stoffel: They can undergo more frequent breast cancer screening, colonoscopy, or endoscopic ultrasound or MRI of the pancreas. They can also start sooner to change behaviors (like stopping smoking) to decrease their cancer risk.
The bottom line: While most pancreatic cancers are not associated with an inherited risk, 1 in 10 are, and those can sometimes be discovered through genetic testing.
Family history alone may not be enough; every pancreatic cancer patient should have a conversation with his or her doctor about genetic testing.
