Cancer & Male Infertility
IN THIS SECTION:
Male Reproductive System | Surgery | Radiation | Chemotherapy | Sperm Banking
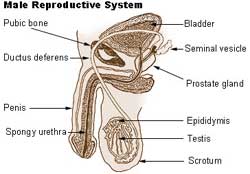
Male Reproductive System
The testicles are the male reproductive organs. Coiled within each testicle are the seminiferous tubules. The seminiferous tubules are lined with spermatogonia cells. These are cells that produce sperm. Semen is the fluid that a man ejaculates. Sperm are found within semen and are the cells that fertilize a female's egg resulting in pregnancy. The ability to produce sperm is dependent on adequate levels of hormones, called FSH (follicle stimulating hormone) and LH (luteinizing hormone). LH and FSH are released by the pituitary gland, located in the brain.
Testosterone is the male hormone responsible for secondary sexual characteristics (facial hair, deep voice, mature genitalia) and maintaining normal male sexual function. Testosterone is produced by Leydig cells, which are found throughout the testicle.
Surgery
Some surgical techniques used for primary cancer control will result in sterility. This may be the result of removal of organs necessary to make or transport sperm. Surgery that involves the male reproductive organs such as removal of both testicles, the prostate gland or the bladder will result in infertility. Damage to the nerves in the pelvic area may result in the loss of ability to ejaculate. Retroperitoneal lymph node dissections may result in retrograde (backward) ejaculation making conception difficult.
Radiation
Radiation therapy can cause infertility in two distinct ways:
Primary testicular damage occurs from radiation aimed directly at or near the testicles. Spermatogonia (sperm forming) cells are extremely sensitive to the effects of radiation therapy. Doses as low as 600 cGy cause irreversible damage to the sperm forming cells. Doses less than this may cause a temporary drop in the number and quality of sperm produced.
The type and dimensions of cancer determine the area of the body to be radiated and how much radiation will be given. For example, radiation may be delivered directly to the testicles, as is used for treatment of testicular leukemia and as part of the total body irradiation used in bone marrow transplant.
Scatter radiation is the term used to describe radiation that occurs in areas not directly within the treatment field, but near to it. Examples of radiation sites that may result in scatter radiation to the testis include: radiation to the lymph nodes in the lower abdomen used for treatment of higher stage Hodgkin's Disease or testicular cancer, or radiation delivered to the upper thigh for a tumor located in this area. Lead shields are used to protect the testis when the treatment field is nearby, but small amounts of radiation exposure may still occur.
Leydig cells are relatively resistant to the damaging effects of radiation therapy. Normal function remains following exposure or treatment with doses less than 2400cGy. This is important because Leydig cells produce testosterone, which is required for normal sexual development and normal sexual activity.
Secondary or indirect testicular failure may occur following radiation therapy to the brain. Radiation may damage the pituitary gland, located in the brain, which is responsible for secreting hormones needed for normal sexual function. Pituitary damage may result in low doses of the hormones (FSH and LH) needed to stimulate the sperm forming cells and Leydig cells. Both LH and FSH are produced in the brain by the pituitary gland. High levels of radiation to the brain can damage the pituitary gland, resulting in an inability to produce the hormones FSH or LH. This in turn causes infertility and low testosterone levels.
Chemotherapy
Sperm forming cells may be adversely affected by chemotherapy drugs. Certain drugs have a much greater chance of causing azoospermia (the absence of sperm in the semen) than others.
The alkylating class of chemotherapeutic drugs has the most significant effect on fertility. Other classes of drugs are generally less toxic to sperm forming cells, but may also cause infertility, especially when used in combination with other drugs.
- Busulfan
- Carmustine (BCNU)
- Chlorambucil
- Cisplatin
- Cyclophospamide
- Lomustine (CCNU)
- Melphelan
- Nitrogen Mustard
- Procarbazine
- Temozolomide
- Thiotepa
- Vinblastine
The total dose of chemotherapy drug is an important determinant of potential damage. Not surprisingly, the higher the total dose, the more potential for damage to the sperm forming cells. Combinations of drugs may result in infertility at lower total doses.
Leydig cell function, which is necessary for testosterone production and normal sexual functioning is much more resistant to the effects of chemotherapy, and is rarely affected by chemotherapy alone.
It is very difficult to predict exactly which men will experience permanent sterility following chemotherapy treatments. Individual issues, such as pre-cancer fertility and the influence of the cancer itself, in addition to the therapy, play an important role.
Men with some types of cancer will have abnormal sperm counts even before treatment is started. About one-half of men with testicular cancer and about 40% of men with Hodgkin's disease have low sperm counts at the time of diagnosis.
Sperm Banking
Semen cryopreservation is the technical name for sperm banking. Sperm banking is the cooling and storage of sperm at very low temperatures (-196 degrees centigrade) for a prolonged period. Men may choose to bank sperm if there is a possibility of losing fertility. This is an important option for men who have not established a family or whose family is not yet complete. Assisted reproduction techniques are medical procedures that help infertile couples achieve pregnancy. Using these methods, pregnancy can occur using frozen semen samples that have very low numbers of sperm. For this reason, all men who hope to father a child in the future should consider cryopreservation of semen or testicular tissue, even if the specimens have low numbers of sperm.
Please see our page on the Emotional Aspects of Sperm Banking and Sperm Banking Procedure for more information.