Cancer Scientists of the Future
By Beth Uznis Johnson

Strong mentorship and sponsorship leads to promising careers
Elizabeth Lawlor, M.D., Ph.D, believes that stronger lines of communication between cancer disciplines are one important way to expedite the translation of research discoveries into the clinic.
After all, discoveries that are impactful in the lab are not impactful to society until a drug, for example, is developed and approved by the Food and Drug Administration and made available to patients. This process takes years and ultimately requires a change in clinical practice if broad impact is to be realized.
“People who do cancer research include those who work with the very smallest molecules and cells, to those studying entire populations of individuals. These researchers speak very different languages and have very different backgrounds,” says Lawlor, former-associate director for education and training at the Rogel Cancer Center. “The best time for cancer researchers to learn how to communicate with one another is during their training.”
One especially important aspect, she adds, is mentorship of the next generation of cancer scientists. With more than 500 researchers at the Rogel Cancer Center, nearly everyone does some sort of mentoring of emerging physicians or scientists.
“As mentors, it is critical that we impart not only knowledge in our own specific area of research, but also how to collaborate across disciplines to move science forward. Mentoring is inherent in what we do every day,” Lawlor says.
Reshma Jagsi, M.D., D.Phil., can attest to the strong mentorship program in radiation oncology at Michigan Medicine. Mentored as a junior researcher by Lori Pierce, M.D., Jagsi received tenure in 2013 and now conducts breast cancer research across the spectrum of care in addition to research in health services, cancer care delivery outcomes, bioethics and gender equity in the medical profession.
Jagsi now mentors Christina Chapman, M.D., who she describes as “the type of talent our field is going to benefit from in the future.” Chapman wanted to research whether black women might benefit from different breast screening guidelines, and Jagsi connected her with an external contact, which led to Chapman receiving NIH funding to execute the project.
And, she linked Chapman with the Michigan Radiation Oncology Quality Consortium to further her work in racial disparities in breast cancer treatment. Pierce is also involved in MROQC, bringing together three generations of radiation oncology mentorship.
“I studied career development in medicine and it opened my eyes to the importance of mentorship and helping someone articulate their goals and what skills they need to build,” Jagsi says.
From undergraduate and graduate students to post-doctoral researchers and beyond, the Rogel Cancer Center aims to provide venues and opportunities for research trainees to speak to each other, learn through mentorship, identify gaps in knowledge and work together to fill those gaps.
The cancer center has six training grants funded by the National Cancer Institute that target very specific groups of trainees.
“Research education and training is integral to all aspects of our mission, and we fund it through a diverse array of sources that range from federal grants to philanthropy. The transdisciplinary aspect of our training experience here at U-M is key and what sets us apart,” Lawlor says.
Here are some examples of the productive scientific partnerships between mentors and mentees working to advance cancer science at the Rogel Cancer Center.
Quality nursing care begins with informed science
The National Academy of Medicine has cited a shortage of both oncology nurses and nursing faculty. Christopher R. Friese, Ph.D., R.N., associate director for cancer control and population sciences at the Rogel Cancer Center, believes a solution to bridge the gap starts with bringing oncology nurses into the workforce with expertise in both clinical work and research.
“You can’t have high quality nursing care without high quality nursing science to inform that practice. It’s clinically informed science and scientifically informed clinical practice,” says Friese, Elizabeth Tone Hosmer Professor of Nursing and professor of health management and policy at the University of Michigan.
The University of Michigan School of Nursing offers a three-year Ph.D. program involving rigorous coursework in research methodology and theory. Doctoral students are paired with a faculty mentor and embedded into a funded research team throughout the program.
“Being able to mentor the clinical nursing staff and think about their advancing careers, or help them answer tough questions on the floor and apply the evidence base we have, and seeing the problems that patients and nurses and doctors face is very valuable,” Friese says. “We are then able to bring that back to my research team to systematically study it and improve it. It’s a really nice synergy.”

Alex J. Fauer, R.N., is a third-year student who moved into the Ph.D. program directly from U-M’s bachelor of science in nursing program. He was a part of Friese’s team from day one to begin mastering the practice of research and learning the methods and theory he’d need in order to launch his own research in the future.
“I was confident that Chris would be a strong mentor to help me develop my skillset in quantitative cancer care delivery research and health policy,” Fauer says. The two had worked together during Fauer’s undergraduate studies on a grant to study hazardous drug exposures for nurses. Fauer presented findings on chemotherapy spills to the Oncology Nursing Society.
In the Ph.D. program, Fauer is part of Friese’s research team to assess the impact of communications and technology use on health care quality in outpatient chemotherapy centers across Michigan. Fauer led visits to eight clinical practices to observe clinical care; he interviewed doctors, nurses and patients about their experiences to get a better understanding of opportunities to improve communication.
“About 7% of patients in the study had to go to the ER or have unscheduled clinic visits to manage their side effects,” Friese says. “There’s an important opportunity there to prevent toxicities from getting so bad that they need extra aggressive treatment.”
Friese says a goal of his mentorship is to demonstrate to Fauer that you can remain clinically grounded as you launch a research program.
In 2019, Fauer received a prestigious American Cancer Society Doctoral Degree Scholarship and is immersed in the data analysis phase of his dissertation to understand the patient experience with care and health care utilization among older adults diagnosed with leukemia and lymphoma.
Fauer will join the National Clinician Scholars Program at UCLA as a postdoctoral fellow after completion of his Ph.D.
Meanwhile, Friese’s team continues work on technology and communication in medical oncology practices across Michigan, among other projects. His team also received an education training grant from the National Cancer Institute that funds full-day workshops on chemotherapy safety training for nurses and pharmacy teams.
Collaboration to uncover the complexities of pancreatic cancer
Pancreatic cancer is one of the deadliest human malignancies, with a five-year survival rate still in the single digits. But pancreatic cancer researchers do have scientific reason for hope, as the five-year survival rate, though low, has recently doubled.
This is where mentorship and team science come in.
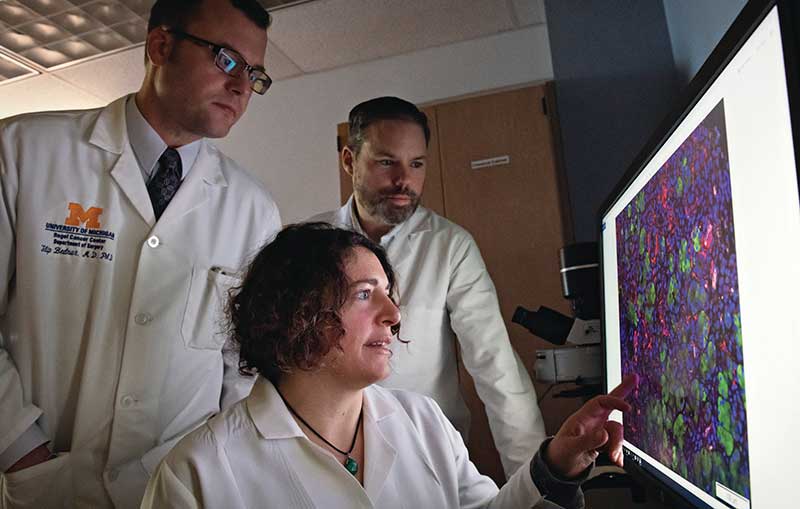
Timothy Frankel, M.D., assistant professor of surgery at Michigan Medicine, studies tumor immunology as it pertains to pancreatic cancer. His focus is on both immune resistance to cancer and parts of the immune system that may cause it.
Filip Bednar, M.D., assistant professor of surgery at Michigan Medicine, was drawn to the epigenetic regulation of the pancreatic tumor microenvironment because there is much to learn about the biology of this complex disease.
Both scientists are mentored by Marina Pasca Di Magliano, Ph.D., associate professor of surgery and cell and developmental biology at Michigan Medicine. She believes science is shifting to a team enterprise so that, while individual researchers are moving toward the next steps in their careers, teams can engage in complementary work to move science forward faster.
“I mentor junior faculty, graduate students, undergrads and postdocs. If people have mentorship they will do well. It is much more efficient if you don’t make the mistakes others before you have made,” Pasca Di Magliano says.
And, she adds, she learns just as much from the scientists she mentors as they learn from her.
“The work that’s being done feeds in to a lot of different clinically relevant aspects of pancreatic cancer,” Bednar says. “We’re going to potentially, as a group, contribute new information in screening and early diagnosis. In terms of treatment, all of us are working on different aspects of understanding how the immune system works or doesn’t work in pancreatic cancer.”
In her research to pursue mechanistic studies to dissect the cellular cross-talk in the pancreatic cancer micro-environment, Pasca Di Magliano saw an opportunity to move from mouse models to human samples.
She has been instrumental in collaborative efforts to build a pipeline to perform single-cell sequencing and mass cytometry on pancreatic tumor samples and matched blood, as well as pancreatitis and healthy blood.
“We are sequencing all the different tumor cells in the microenvironment,” she explains. “We are mapping how they’re interacting with one another and can see what genes tumor cells have and what genes immune cells have.”
Initial analysis has revealed a profound difference in the immune composition of peripheral white blood cells in pancreatic cancer patients versus healthy individuals. The pancreatic research team hopes to follow patients over the long term post-treatment, as well as identify at-risk patients.
Bednar and Frankel agree that Michigan Medicine and the Rogel Cancer Center are a great place to build a career focused on academics blended with clinical care. In addition to labs in close proximity that allow for close collaboration, the Department of Surgery requires contracts for surgeon scientists that name both a clinical mentor and basic science mentor.
“More and more through the years, our labs almost run seamlessly, but there are fringe elements that are independent,” Frankel says. “The further along I move in my career, it’s starting to shift from mentor to colleague. As that happens, Marina will mentor me to become a mentor.”
Striving for social justice and health equity
Anyone with an interest in disparities research understands the constant struggle with sample sizes. Most studies in the 1970s and ‘80s in the United States did not have racial or ethnic diversity. For young disparities researchers starting careers, finding mentorship can also be challenging, as many in this field are often from minority backgrounds who are -- by definition -- underrepresented.

That didn’t stop Jagsi, Newman Family Professor and deputy chair of radiation oncology at Michigan Medicine, from pursuing research on disparities, bioethics and gender equity.
One of her first large research grants was to study career development in medicine.
“That opened my eyes to the importance of mentorship. I began studying it and wrote papers on the power of mentor networks and sponsorship,” Jagsi says.
Mentorship, she says, is helping someone articulate their goals and build the skills they need to address their research problems. Sponsorship is more about putting your own reputation on the line to give a protégé a chance to shine.
It was one of Jagsi’s own mentors, a former professor from Harvard who was serving as a visiting professor, who encouraged her to work with Christina Chapman, M.D., who was then a resident and is now a faculty physician-researcher at Michigan Medicine and the VA Ann Arbor Healthcare System. They met to discuss, among other things, Chapman’s interest in using simulation modeling to investigate whether African American women should have breast cancer screening guidelines different than the overall population.
“Christina was ready to dive into a data set and discovered there were no data sets of screening trials that contain sufficient numbers of African American women to actually investigate the important topic she had identified as a research question,” Jagsi says.
Jagsi introduced her to an investigator at Georgetown University for the information she needed. Chapman brought forward suggestions and later wrote about ways to better promote equity in physician graduate medical education. They have been mentor and mentee ever since.
“Dr. Chapman is a warrior fighting health injustice,” Jagsi says. “She completely appreciates that social determinants of health far outweigh the influence of factors like medical care. She’s drawing her inspiration and strength from individual patient encounters and enriching her work because of them.”
Chapman served as a discussant on a panel on workplace inequities at the 2019 American Society of Clinical Oncology’s annual meeting in Chicago. She continues her research on whether black women will benefit from different breast cancer screening guidelines since they’re diagnosed at a younger age and get more aggressive subtypes.
“I love seeing patients as a radiation oncologist and performing research, and cannot think of a better career to have pursued,” Chapman says. “However, when I think about my overarching life goal, it is broader than my career and more about advancing social justice. Research is a means to do that, and continuing to see patients and continually being made aware of the challenges discrimination poses for many in academia drives a lot of the questions I ask.”
An annual research training symposium provides opportunities for trainees to present research in progress. There are also several Cells to Society seminars each year for investigators to present high-level overviews of pressing issues in cancer research, from cell biology to population sciences. Presenters cover different perspectives on the issue.
Visit our Education and Training webpages for more information.
Learn more about the Rogel Cancer Center members who are mentoring future scientists
Continue reading Illuminate 2020 or print the 2020 issue
Get research news in your inbox!
Our Illuminate e-newsletter showcases the important and unique research underway at the Rogel Cancer Center.
Follow this link and sign-up today!
