When It’s Not Exactly Cancer: Renaming Early Stage Thyroid Tumors
Media contact: Nicole Fawcett, 734-764-2220 | Patients may contact Cancer AnswerLine, 800-865-1125
Categorizing non-life-threatening thyroid tumors separately from more aggressive thyroid cancers could change patients’ lives for the better, researchers say.
ANN ARBOR, MICH -- The number of people diagnosed with thyroid cancer is increasing -- one of the few cancers for which this is still the case. But a subset of these patients may be getting overdiagnosed with cancer.
A study out today in JAMA Oncology suggests reclassifying a slow-growing, not-life-threatening type of thyroid nodule to eliminate the stigma of diagnosing someone with cancer. The recommendation also includes less-aggressive therapy for these patients.
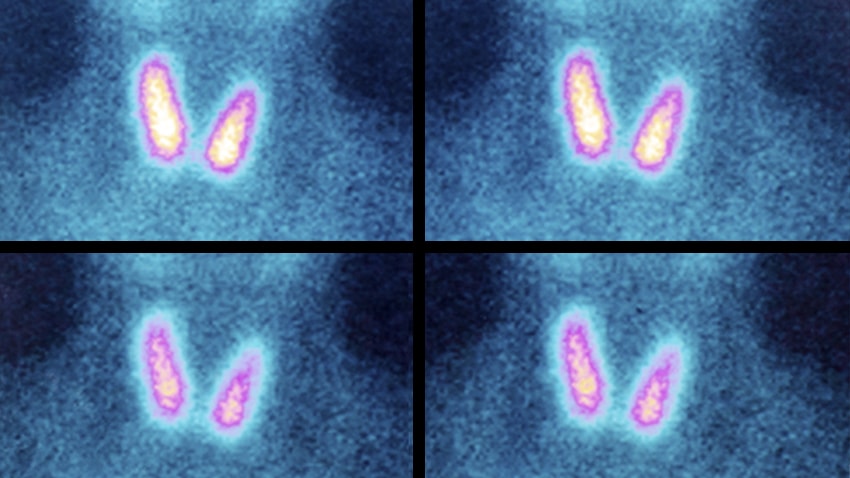
An international working group of 24 pathologists reviewed 109 patients with noninvasive encapsulated follicular variant of papillary thyroid carcinoma. They found that all of the patients were alive with no signs of cancer up to 26 years later.
The working group suggests renaming this type of thyroid cancer noninvasive follicular thyroid neoplasms with papillary-like nuclear features, or NIFTP.
"When you think of how many people have thyroid nodules and how often this comes up, it's not a trivial impact," says study author Thomas J. Giordano, M.D., Ph.D., director of molecular and genomic pathology at the University of Michigan. The authors estimate reclassifying this tumor could impact more than 45,000 patients worldwide each year.
We talked to Giordano about the difference a name might make -- both for physicians and patients.
Why rename this diagnosis?
Giordano: Patients with this variant of thyroid nodule did extremely well over an extended period of follow-up. The risk of this recurring or metastasizing is really low -- so low that we found you don't need to do extra treatment, such as removing the entire thyroid or giving radioactive iodine.
While these treatments aren’t extremely toxic, they do cause side effects, including long-term physical impact. There also can be a financial impact for some patients. Radioactive iodine therapy can cost $5,000 to $8,500.
We had a psychiatrist as part of this work group who emphasized the impact of the "C-word." It can’t be understated for patients. One of our endocrinologists has attended support group meetings here and found a patient with the worst kind of thyroid cancer sitting next to someone with this indolent version. This patient thinks he has the same disease, and feels he needs the same degree of support. Is it fair to make that person feel like a "cancer survivor"?
The paper talks about a phenomenon of cancer overdiagnosis. Why are we seeing this?
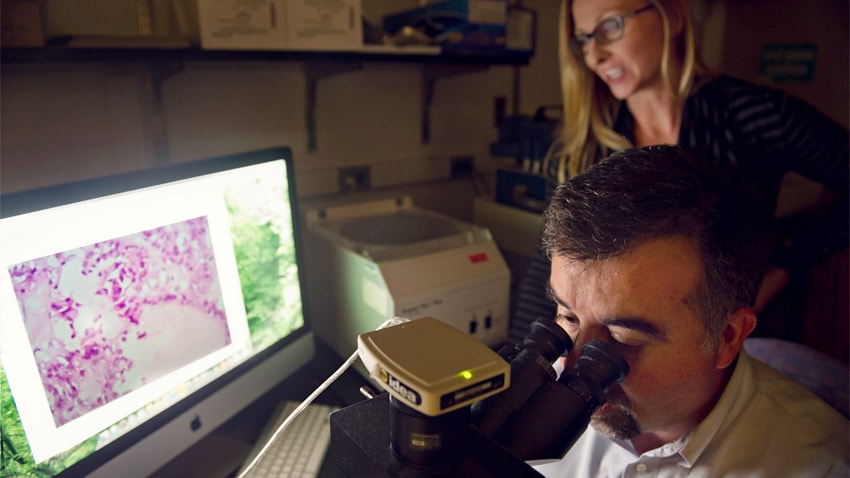
Thomas J. Giordano, M.D., Ph.D.
Giordano: Thyroid cancer is a prime example of cancer overdiagnosis. It is one of the few cancers where incidence is going up. Partly that’s because people have looked harder. They're screening for it. Also, over time, the threshold for pathologists to call a nodule cancer has steadily gone down. Thyroid nodules are common. But a lot of them are indolent and would never become a problem. When it's found, though, patients undergo what might be unnecessary treatment, expense and long-term physical and psychological burden.
Is this an issue in other cancer types, too?
Giordano: These slow-growing nodules or lesions occur in all types of tumors. It’s particularly prevalent in the thyroid. We see this in prostate cancer, too. Many prostate cancers would never impact a person's life, but if a urologist finds it through PSA screening, the person gets a prostatectomy or other treatments and all the long-term effects that go with that.
In the oral pharynx, we call these tumors dysplasia. In breast cancer, it's ductal carcinoma in situ. Some of these lesions are barely cancer, and these patients tend to do fine. We need better ways of identifying these indolent tumors from the aggressive cancers, and offer patients treatment accordingly.
Will your recommendation change how physicians diagnosis this condition?
Giordano: NIFTP cannot be diagnosed at biopsy, so patients with a suspicious nodule will still need to have a portion of their thyroid removed. We’ve recommended guidelines to help pathologists determine which lesions are invasive cancer and should be treated aggressively, and which lesions are not invasive and should be classified as NIFTP.
What will be the impact on the care of patients with this diagnosis?
Giordano: We're making a strong statement that surgery is sufficient for this tumor. These patients do not need a second surgery to remove the rest of the thyroid and they do not need radioactive iodine therapy. Endocrinologists and surgeons will need to settle on proper follow-up for these patients. As our working group continues to synthesize the data we gathered, we expect additional insights and recommendations for long-term follow-up of these patients.
Learn more about thyroid cancer and outcomes
Thyroid cancer page on mcancer.org
Study: Worse Survival When Specific Thyroid Cancers Spread to Bone
Complications from Thyroid Cancer Surgery More Common Than Believed, Study Finds
Imaging after thyroid cancer treatment does not necessarily mean better outcomes, study finds
