Better Communication, Better Cancer Care
By Shelley Zalewski
Apps, text messaging, other technology keep cancer patients, families and survivors in the know
Every day, University of Michigan Rogel Cancer Center researchers are developing new ways to treat cancer. Genetic testing to identify those at risk. Next-generation imaging to see it. Precision therapies to target it.
They’re also working on new ways to talk about it.
Understanding and treating cancer presents extraordinary communications challenges. Patients can be overwhelmed by information. Providers struggle to bring clarity to complexity. Face-to-face time with clinicians is in short supply. Everyone needs tools to understand their diagnosis and to be understood.
For more than 20 years, developing those tools has been the purpose and passion of the Center for Health Communications Research, also called CHCR, at the Rogel Cancer Center. Cancer clinicians and CHCR experts partner to design and test evidence-based educational and behavior-change interventions. Advances in technology have allowed for the creation of high quality tools using print, mobile device, web-based or other communication channels and strategies.
CHCR is one of more than a dozen shared resources available to researchers at the Rogel Cancer Center. It provides communications expertise and services for research studies requiring targeted and tailored interventions that inform health decisions. The dedicated team of technology experts, behavioral scientists, graphic designers and project managers helps research investigators across a range of services, including:
- Engaging enrollment approaches to optimize trial recruitment
- High quality mobile apps, websites and personalized media
- Behavioral change interventions for investigators conducting research on cancer prevention, control and care delivery
CHCR’s latest projects illustrate the power of technology to improve communication and communication to improve outcomes.

Keeping patients informed and connected
For patients looking for answers and advice about cancer treatment, the challenge isn’t a lack of information. More often they find themselves overwhelmed by online searches and overloaded with brochures and handouts.
“It’s not just too much information; it’s often the wrong information,” says breast cancer surgeon Michael Sabel, M.D., division chief and William W. Coon Collegiate Professor of Surgical Oncology at Michigan Medicine. “Even when the source is reliable (and many on the web are not), it may not address the patient’s specific concern. As clinicians, we wish we could be there 24/7 to answer questions and troubleshoot issues.”
While there’s no substitute for a one-on-one discussion with a doctor or nurse, Sabel worked with CHCR to develop the next best thing, launching the Breast Cancer Ally mobile app.
Unlike health apps that provide only generic medical content, Breast Cancer Ally asks patients specific questions about their disease stage, treatment plan, symptoms and concerns, and then delivers customized, actionable information. Patients recovering from axillary lymph node dissection are prompted with instructions and reminders to perform arm exercises to improve mobility, while patients undergoing chemotherapy receive tips for managing side effects.
“The app is a clinical companion,” says Sabel, “enhancing doctor-patient interaction, not replacing it.” Sabel is collaborating with CHCR and other Michigan Medicine partners to develop the next generation Breast Cancer Ally and extend the platform to other cancer types.
“For an even more personalized, just-in-time connection with patients, we’re linking to our electronic health information system and adding text messaging functionality,” he explains. The goal is to make the app an even more powerful, responsive tool to manage treatment-related side effects before they become serious complications.
Overcoming obstacles to coordinated care
After initial breast cancer treatment, the focus shifts to survivorship care. Patients need both ongoing surveillance and preventive care, as well as support to manage late effects and cope with the psychosocial effects of their cancer.
Team-based cancer care, with well-defined roles and good communication between the oncologist, primary care physician and patient, is the recommended approach to maximize quality and improve outcomes.
But it can be tough to keep patients and providers on the same page. With funding from a K07 award from the National Cancer Institute, investigators from the U-M Cancer Surveillance and Outcomes Research Team, known as CanSORT, are collaborating with CHCR to pilot a first-of-its-kind intervention that facilitates team-based breast cancer survivorship care.
The project is led by Lauren Wallner, Ph.D., MPH, assistant professor of general medicine and epidemiology at the University of Michigan, and CanSORT co-directors Steven Katz, M.D., MPH, professor of medicine and health care management and policy, and Sarah Hawley, Ph.D., MPH, professor of general medicine, health care management and policy, health behavior and health education.
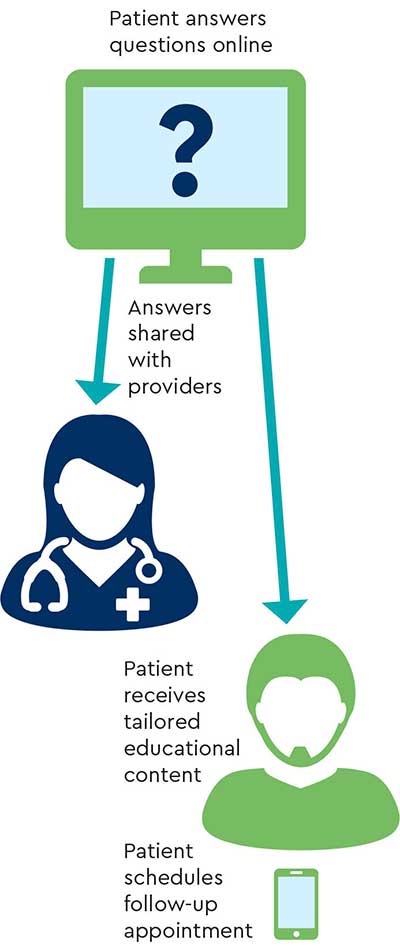
The intervention is powered by a patient- and provider-facing, interactive web-based tool called ConnectedCancerCare. On the website, patients answer questions about treatment and care experiences, provider references, concern about recurrence and more. They then receive tailored educational content, including tips on what to expect from and how to communicate with their PCP and oncologist about what happens next with survivorship care. They can learn about regional and national resources for common concerns like financial matters, managing side effects and coping. And they are prompted with email or text reminders to schedule appointments with their primary care physician.
The tool also communicates with the PCP and oncologist, generating letters highlighting the patient’s preferences, flagging top concerns and identifying knowledge gaps about provider roles and services.
Surveys conducted three months into a pilot randomized trial reveal high user satisfaction with the tool. Compared with the static survivorship intervention provided to the control group, ConnectedCancerCare was shown to improve provider communication with patients. Patients using it were more likely to schedule guideline-concordant PCP follow-up appointments.
The next step is a large, multi-center trial to evaluate ConnectedCancerCare in general oncology practice settings nationally.
Safeguarding the health of our most valuable partners
Patients undergoing hematopoietic cell transplantation -- commonly referred to as blood and marrow transplant or BMT -- are among the most vulnerable patient populations.
These fragile patients are wholly dependent on family caregivers, such as spouses, parents, friends or other nonmedical caregivers, throughout their rigorous therapy and journey, starting during the initial hospital stay and continuing well beyond their return home.
In 2014, pediatric hematologist Sung Won Choi, M.D., Edith S. Briskin and Shirley K. Schlafer Foundation Research Professor of Pediatrics at Michigan Medicine, began working with CHCR to develop and test BMT Roadmap, a web-based tool to help caregivers navigate inpatient BMT treatment. Her work was directly informed by her studies of BMT patients enrolled in clinical trials, where she recognized the need to also support the family caregivers upon whom patients were completely dependent during their care.

By leveraging mobile health, or mHealth, technology, her goal was to make care and monitoring easier by providing real-time patient lab results, medication lists, clinical trial details, a photo directory of the health care team, a detailed description of the transplant process, and a discharge checklist, all in one place -- at the touch of a screen. This mHealth tool is now being expanded to support caregiving after discharge, where the majority of caregiving takes place without the daily supervision of the health care team.
With the next generation of BMT Roadmap, Roadmap 2.0, Choi turned her attention to an unmet need she encountered every day: amid the myriad needs of their recovering loved ones, caregivers often neglected to look after themselves, and in turn, may be overlooked or become ill.
“Caring for a transplant patient takes a physical and emotional toll,” says Choi. “Healthier, more resilient caregivers are more likely to make a positive impact over the long journey of transplant and recovery. We need to give them the tools to stay well throughout that journey.”
Roadmap 2.0 will be a phone-based mHealth app. To determine the design and features of Roadmap 2.0, Choi’s research team interviewed more than 50 patient-caregiver pairs and will combine those insights with data from a national caregiver health survey that captured more than 1,300 BMT caregiver respondents.
An NIH grant funds the project, which will be evaluated with a randomized clinical trial. With collaborators across Michigan Medicine, the team’s goal is to leverage mHealth and integrate clinical, physiological and biological data to better understand caregiver health, and how that may ultimately impact patient health.
Colon cancer screening: turning intention into action
Face it: no one is thrilled about colorectal cancer screening.

Breaking down barriers to screening is the goal of Ken Resnicow, Ph.D., Irwin M. Rosenstock Collegiate Professor of Public Health and associate director for Community Outreach, Engagement and Health Disparities at the Rogel Cancer Center. Resnicow and CHCR collaborators Larry An, M.D., and Sarah Hawley, Ph.D., MPH, have developed a texting intervention to encourage people in need of or overdue for colon cancer screening to take the next step.
The collaborative effort began when the National Cancer Institute created and deployed a text message-based program to promote cancer prevention and control behaviors of healthy diet, exercise and smoking cessation. Through collaboration with U-M in 2017-18, NCI provided the messages to CHCR, who updated the information using local technology. The rebranded U-M program is called Tips4Health and is now offered throughout Michigan with good uptake.
Yet one limitation of the program was that it wasn’t individualized to users; everyone got the same messages that were developed by the NCI. And the original suite of programs from NCI -- healthy diet, exercise and smoking cessation -- did not address a key need of the U-M catchment area, specifically, to improve uptake of colon cancer screening.
Based on existing colorectal cancer screening programs developed by Resnicow, Hawley and the CHCR team, colorectal screening messages were added to Tips4Health, tailored to individual users’ knowledge, preferences and barriers to getting screened.
Users are prompted to identify the barriers that make them reluctant to undergo screening. For example, barriers to colonoscopy can include aversion to the preparation, fear of sedation, concerns about missing work or having to bring along a driver.
Tips4Health-CRC Screening now provides content to address each barrier. Additionally, the team reached out to colleagues at Virginia Commonwealth University and Temple University, who had developed tailored video testimonials designed to help patients overcome specific concerns about colon cancer screening. The testimonials were shared with U-M researchers and added to Tips4Health so users of the app receive text messages with optional video links.
“We’re working toward adding ‘click to schedule’ capability to make a colonoscopy appointment, or the delivery of an at-home test kit (e.g., ColoGuard®) on the spot,” says Resnicow. “That’s the final step in turning intention into action.”
Bridging the information-comprehension divide
Research shows that patients retain only about a third of what’s discussed in a typical doctor visit. So for an overwhelmed patient presented with a cancer diagnosis and asked to evaluate complex treatment options, it’s likely even less.

A team led by CHCR co-directors Larry An, M.D., and Sarah Hawley, Ph.D., MPH, has been working with U-M engineering professor Rada Mihalcea, Ph.D., to leverage technologies like artificial intelligence (AI) and natural language processing (NLP) in next-generation doctor-patient interventions. These technologies use algorithms to understand human speech.
“AI and NLP help people interact with technology the same way we interact with each other -- by speaking and listening, not pointing and clicking,” An says.
An’s moment of realization about AI’s potential came at a symposium hosted by Mihalcea where they met Scott Huffman, vice president of engineering at Google, who is responsible for the company’s AI-based virtual helper, Google Assistant.
“People are welcoming agents like Google Assistant, Amazon’s Alexa and Apple’s Siri onto their phones and into their homes because they make life easier,” An says. “Could they make it easier for cancer patients to comprehend, retain and act on information from clinic visits?”
Encouraged by Huffman, they applied for and earned a Google Focused Award to find out. The awards are for research in areas of key interest to Google, as well as the research community. They are unrestricted gifts that typically last for two to three years. Recipients have the advantage of access to Google tools, technologies and expertise.
Still in its infancy, their trial (targeted for early 2020) will put a cancer-trained version of Google Assistant on a patient’s smartphone or other device. In the consult room, it will listen, record and transcribe. At home, the patient can search the transcript to revisit specific issues (“What did the doctor say about my lymph nodes?”), navigate cancer terminology (“What are lymph nodes, anyway?”) and more.
Clinicians across the Rogel Cancer Center have shared even more possible applications for the Assistant. The technology could help prepare patients for clinic visits, learning their top concerns in advance and ensuring they are addressed. It could also improve inpatient unit communications, when coordinating dialog between patients, rounding specialists and visiting family members is challenging.
“When patients don’t retain information, much of the value of health care leaks away,” says An. “AI has the potential to restore that value on demand.”
Learn more about the Center for Health Communications Research and the researchers in this article
Continue reading Illuminate 2020 or print the 2020 issue
Get research news in your inbox!
Our Illuminate e-newsletter showcases the important and unique research underway at the Rogel Cancer Center.
Follow this link and sign-up today!
