Blood Cancer Research
The latest research on blood cancer detection, diagnosis and treatment
Researchers Achieve Elimination of Leukemia and Lymphoma Tumors in Mouse Models
A potent and selective degrader of the transcription factor STAT3 offers a new approach to a previously “undruggable” target
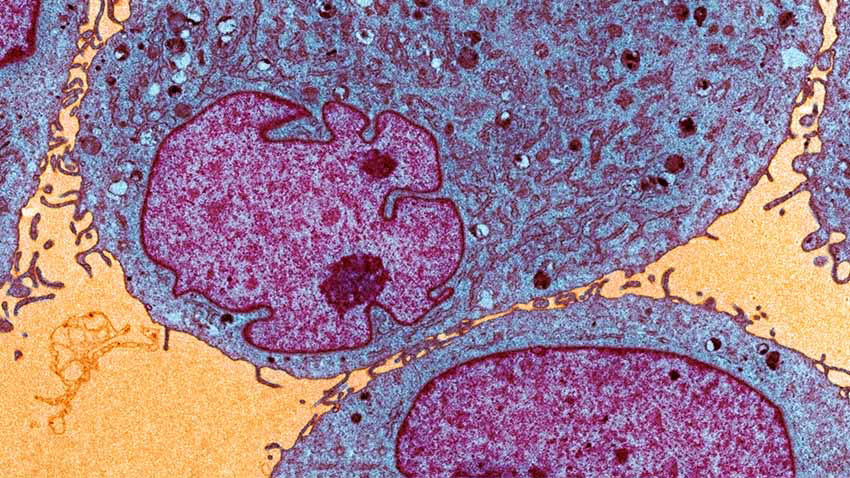
For decades, a transcription factor known as STAT3 has been a major therapeutic target in the treatment of cancer. But STAT3 has largely been considered “undruggable” due to the difficulty of developing compounds to effectively inhibit its activity.
Researchers at the University of Michigan Rogel Cancer Center have taken a promising new approach to targeting STAT3 -- developing a small-molecule compound that harnesses the power of a natural cellular “cleanup” system to get rid of it entirely, rather than traditional methods that have tried to block its action.
The U-M compound was able to achieve long-lasting and nearly complete elimination of tumors in mouse models of leukemia and lymphoma, the authors report in Cancer Cell.
In a mouse model of leukemia, the degrader eliminated all of the tumors, with the mice remaining tumor free for 60 days. In two mouse models of lymphoma, the drug eliminated all of the tumors for more than 100 days, when the experiments were ended. The compound was well-tolerated by the mice, the researchers note.
“STAT3 plays a major role in almost every aspect of human cancer -- in cancer initiation, progression, metastasis and immune evasion,” says study senior author Shaomeng Wang, Ph.D., the Warner-Lambert / Parke-Davis professor and a professor of internal medicine and pharmacology at the U-M Medical School, and a professor of medicinal chemistry at the U-M College of Pharmacy. “It also has been implicated in autoimmune and inflammatory diseases. So, there’s a lot of therapeutic potential if one can target STAT3 successfully.”
Applying a technology called proteolysis-targeting chimeras (PROTAC), the investigators designed the compound to specifically tag the STAT3 protein for recycling by the body’s own cleanup systems. This eliminates the STAT3 protein from cells and tissues and blocks its activity entirely, while leaving the function of related proteins intact.
This new approach circumvents problems seen in drugs aimed at merely inhibiting STAT3’s activity, including the accidental targeting of other proteins in the seven-member STAT family, which mediate many aspects of cell growth, differentiation and death, says Wang.
The study’s co-first authors are Longchuan Bai, Ph.D. and Haibin Zhou, Ph.D., two research scientists in Wang’s lab, Renqi Xu, Ph.D., a postdoctoral fellow in Wang’s lab, and Yunjun Zhao Ph.D., a former postdoctoral fellow in Wang’s lab and currently a professor in Shanghai, China.
The research team, which included collaborators at the U-M Life Sciences Institute’s Center for Structural Biology and the College of Pharmacy’s Pharmacokinetics and Mass Spectrometry Core, has since further optimized the compound described in the study into a clinical development candidate.
“In the clinical setting, we hope to be able to achieve a dosing schedule that is convenient for cancer patients, perhaps requiring administration of the drug as little as once a week based upon our study,” Wang says.
The group is collaborating with Oncopia Therapeutics, a U-M start-up company, to complete studies required for filing an investigational new drug application with the Federal Food and Drug Administration, which is required to initiate human clinical trials.
The study was funded by a research contract from Oncopia Therapeutics and by the Rogel Cancer Center Core Grant (P30 CA046592) from the National Cancer Institute, part of the National Institutes of Health. The research used resources of the Advanced Photon Source at the Argonne National Laboratory and was supported by the Michigan Economic Development Corporation and the Michigan Technology Tri-Corridor (Grant 085P1000817).
For disclosure, U-M has filed patent applications on the compound and its analogs. These patents have been licensed by Oncopia Therapeutics, in which Wang is a co-founder, a paid consultant and owns stock. U-M also has a financial interest in Oncopia.
Additional authors on the paper include Krishnapriya Chinnaswamy, Donna McEachern, Jianyong Chen, Chao-Yie Yang, Zhaomin Liu, Mi Wang, Liu Liu, Hui Jiang, Bo Wen, Jennifer L. Meagher, Duxin Sun and Jeanne Stuckey, all of U-M.
Improving Bone Marrow Transplant Patient Outcomes
While it plays a protective role in other diseases, knocking out NLRP6 in mice led to better outcomes, less-severe symptoms after bone marrow transplant
A protein that protects people with inflammatory bowel disease has quite a different effect in graft-vs.-host disease, a common and challenging side effect of bone marrow transplants.
In a surprising finding, researchers at the University of Michigan Rogel Cancer Center showed the protein NLRP6 aggravated the difficult symptoms of gastrointestinal graft-vs.-host disease (GVHD). Knocking out this protein in mice led to significantly better survival and less severe GVHD.
GVHD, a response to the donor bone marrow, causes symptoms similar to ulcerative colitis, including diarrhea and abdominal pain. Generally, the mechanisms that cause colitis overlap with those that cause GVHD, and many of the treatments are similar.
Studies have shown NLRP6 lessens symptoms in colitis. So when researchers looked at NLRP6’s impact on GVHD, they assumed it would also be protective.
“There are a lot of reasons NLRP6 seemed to work well in those other diseases, but in the case of GVHD, it seemed to do the opposite. In mice where we knocked out NLRP6, instead of doing worse, they did better. That was a big surprise,” says co-senior study author, Pavan Reddy, M.D., deputy director of the Rogel Cancer Center and division chief of hematology/oncology at Michigan Medicine.
In their study, published in Nature Microbiology, the team compared mouse models expressing NLRP6 and those in which the protein was eliminated. In both models, the mice had undergone a bone marrow transplant.
The second surprise was that NLRP6 played a role that was not dependent on microbiome composition. Previous data had suggested NLRP6’s protective role is directly related to the microbes within the intestinal tract: the more good microbes, the more protective effect.
In this study, researchers measured the levels of various microbes, then worked to alter the microbiome, wiping out certain microbes or breeding mice together to share their microbiome. They developed mice in a germ-free environment and then exposed them to a microbiome with and without NLRP6. Each time, those without NLRP6 had better outcomes.
“Even when we did all of those manipulations, the protection was still there in the NLRP6-knockout mice. The composition of the microbiome does not seem to matter, unlike with other disease processes,” says study author Hideaki Fujiwara, M.D., Ph.D., a post-doctoral researcher in Reddy’s lab.
Digging deeper, researchers found a metabolite called taurine that appears to be, in part, responsible for turning on NLRP6 and ultimately making GVHD worse. Changes in the microbiome can lead to excess taurine, which signals NLRP6, which in turn triggers GVHD.
“Just measuring changes in the microbiome is not always sufficient. We have to look at what specifically changes and the consequences of those changes. A change that leads to the generation of metabolites like taurine or other proteins or enzymes will need to be understood to comprehend the effects of the microbiome on GVHD,” says co-senior author Grace Chen, M.D., Ph.D., associate professor of hematology/oncology at Michigan Medicine.
“Conceptually, if we can target this protein and block NLRP6, we can mitigate intestinal GVHD. Or, if you look at it the other way, changing the diet or microbiome to avoid an excessive amount of taurine could be another way to reduce GVHD,” Reddy says.
NLRP6 is expressed in gut cells but not in the tumor cells the researchers studied. This means the bone marrow transplant could do its job to eliminate the tumor. In principle, blocking NLRP6 could limit GVHD without limiting the transplant’s anti-tumor effect.
Reddy notes that no blocker currently exists against NLRP6 and any potential clinical benefit still needs to be explored. His lab plans to follow up with more study of taurine and other metabolites, including how modifying them impacts NLRP6 and GVHD.
Image caption: Drs Fujiwara, Chen and Reddy study research results. Photo credit: Leisa Thompson"
