Previous Forbes Scholars

2019 Forbes Scholars
Collaborative team of Dr. Clifford S. Cho (Surgery) and Dr. Zhen Xu (Biomedical Engineering).
Histotripsy tumor ablation: a trigger to expand the efficacy of cancer immunotherapy

Immunotherapy has revolutionized the outlook for patients with cancers that have some intrinsic visibility to the immune system. Unfortunately, the majority of cancers are largely invisible to immune recognition, and to date, patients with these cancers have not benefited immunotherapy. Histotripsy is a new technology that uses high pressure sound waves to ablate tumors without the need for heat generation or invasive procedures. Importantly, we have discovered that histotripsy ablation of tumors also stimulates a surprisingly powerful immune reaction that triggers tumor rejection. Our project will explore the depths of this potentially revolutionary immune stimulation, measuring its magnitude, identifying its subcellular mechanisms, and characterizing its ability to sensitize previously resistant cancers to immunotherapy.
Clifford S. Cho, M.D.: Biography | Publications
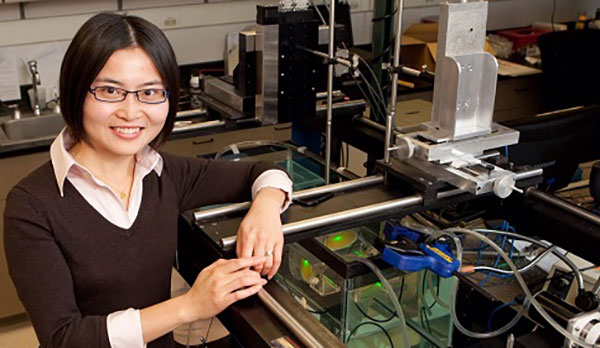
Zhen Xu, Ph.D.: Biography | Publications



Collaborative team of Dr. David Markovitz (Internal Medicine), Dr. Alnawaz Rehemtulla (Radiation Oncology), and Dr. Challice Bonifant (Oncology, Johns Hopkins School of Medicine).
A Molecularly Modified Lectin for Pharmacologic and Immune Therapy of Non-Small Cell Lung Cancer
Certain types of sugar structures are found on malignant cells, such as those from lung cancer, but generally not on healthy human cells. One molecule that is particularly important in lung and other cancers is EGFR, which is apparently coated with these abnormal sugars in tumors. We have molecularly modified a sugar-binding protein from bananas, making it safe while leaving potent sugar-binding activity, and find it to be a very promising therapy in the laboratory dish and in an animal model of lung cancer. It attacks EGFR and destroys it, even in lung cancer cells resistant to standard therapy. We here propose to further study the efficacy and safety of this molecule when used as an anti-lung cancer drug. Using very recently developed technology, we will also assess in fine detail the features of the sugar structures on EGFR in healthy and cancer cells that lend specificity, and hence safety, to this drug. Finally, we will use the sugar-binding protein to guide immune cells to lung cancer cells, leading to their destruction at the hands of what have been called "sweet-CARs", after the name of the technology and with a bow to sugars.
David Markovitz, M.D.
Biography
Publications
Alnawaz Rehemtulla, Ph.D.
Biography
Publications
Challice Bonifant, M.D., Ph.D.
Biography
Publications
Collaborative team of Dr. Daniel Wahl (Radiation Oncology), Dr. Sriram Chandrasekaran (Biomedical Engineering), Dr. Jason Heth (Neurosurgery), Dr. Costas Lyssiotis (Molecular & Integrative Physiology), and Dr. Sriram Venneti (Pathology).

Mapping metabolic rewiring in brain tumors in vivo
Our group believes that there may be common metabolic abnormalities that cause treatment resistance in glioblastoma cells regardless of which genetic abnormalities are present. Thus, drugs targeting abnormal metabolism (instead of genetic abnormalities) in glioblastoma might successfully overcome treatment resistance, as they affect most of the cells in the tumor. In this Forbes Institute for Cancer Discovery grant, our group will use a variety of laboratory-based and computational approaches to determine how abnormal metabolism causes treatment resistance in glioblastoma. Much of our effort will focus on one particular metabolic pathway, called de novo purine synthesis, which our prior experiments have implicated as a major cause of treatment resistance in glioblastoma. We will use the opportunity afforded by the Forbes Institute to measure the activity of this pathway in glioblastoma tumors in mice and in human patients and determine if drugs inhibiting this pathway could be useful to treat this difficult disease.

|

|

|
 |
 |
|
Daniel Wahl, M.D., Ph.D. |
Sriram Chandrasekaran, Ph.D |
Jason Heth, M.D. |
Costas Lyssiotis, Ph.D. |
Sriram Venneti, M.D., Ph.D. |
2018 Forbes Scholars

David Ginsburg, M.D.
An Unbiased Screen for Brain Metastasis-Promoting Gene Networks in Human Breast Cancer
Collaborative team of Dr. David Ginsburg (Life Sciences Institute) and Dr. Stephen J. Weiss (Life Sciences Institute).
This project aims to identify genes whose expression modulate the capacity of breast cancer cells to metastasize and proliferate within the brain. To this end, we will profile the transcriptome of a human breast cancer cell line and its specific subclones that preferentially metastasize to the brain in an in vivo mouse model system. We will also perform a whole genome CRISPR/Cas9 screen to select for genes whose modification leads to alterations in metastatic colonization and growth. We anticipate that this unbiased screening strategy will identify novel therapeutics targets for treatment of breast cancer and potentially other malignancies
David Ginsburg, M.D. Biography Publications
Stephen J. Weiss, M.D. Biography Publications
Justin Colacino, Ph.D., M.A., MPH

Targeting Circulating and Disseminated Tumor Cells From Pre-Invasive Breast Tumors
Collaborative team of Dr. Justin Colacino (School of Public Health) and Dr. Dean Brenner (School of Pharmacology)
Breast cancer is traditionally thought to progress through a continuum from normal breast epithelium, to hyperplasia, to atypical hyperplasia, to ductal carcinoma in situ (DCIS), to locally invasive carcinoma, to metastatic disease. There are a building number of studies which, when taken in aggregate, challenge this conventional wisdom of a linear progression to metastasis. Our study will test the hypothesis that systemic tumor cell dissemination precedes local invasion in breast cancer, and that these early disseminated tumor cells have stem cell-like characteristics. By characterizing the timing and biological drivers of breast cancer dissemination, we hope to develop new targets for breast cancer prevention, diagnosis, and treatment.
The funding from the Forbes Institute will allow our team to use state-of-the-art approaches in circulating tumor cell capture and single cell genomics to isolate, enumerate, and characterize circulating tumor cells from patients with pre-invasive breast lesions, such as DCIS. To ensure successful completion of the project, our interdisciplinary team includes Dr. Colacino, an expert in breast stem cells and carcinogenesis, Dr. Brenner, who is an expert in translational carcinogenesis and the biology of the progression of invasive neoplastic disease, Dr. Wicha, an international leader in breast cancer stem cells, Dr. Jeruss, an expert in breast cancer metastasis and treatment, Dr. Kleer, a renowned breast cancer pathologist and expert in mechanisms of breast cancer invasion and metastasis, and Dr. Nagrath, an expert in developing circulating tumor cell capture devices.
Justin Colacino, Ph.D., M.A., MPH Biography Publications
Dean Brenner, M.D. Biography
Tomasz Cierpicki, Ph.D.
Targeting YEATS4 chromatin reader in cancer
Collaborative team of Dr. Tomasz Cierpicki (Department of Medicinal Chemistry), Dr. Jolanta Grembecka (Department of Pathology) and Dr. Venkateshwar Keshamouni (Department of Internal Medicine, Pulmonary and Critical Care Medicine).
YEATS4, also known as a glioma amplified sequence 41 (GAS41), is an epigenetic reader protein involved in recognition of acetylated histones. Emerging studies implicate YEATS4 as an oncogene in non-small cell lung cancer (NSCLC), glioblastoma, colon and pancreatic cancers. In this proposal we plan to identify small molecule inhibitors of YEATS4 with efficacy in mouse models of cancer. The Forbes Institute grant will allow us to facilitate development of YEATS4 inhibitors and support our interdisciplinary collaboration between Dr. Cierpicki, Dr. Grembecka and Dr. Keshamouni within this project. We aim to provide a proof of concept demonstrating that pharmacological inhibition of the YEATS4 histone reader is therapeutically beneficial in cancer.
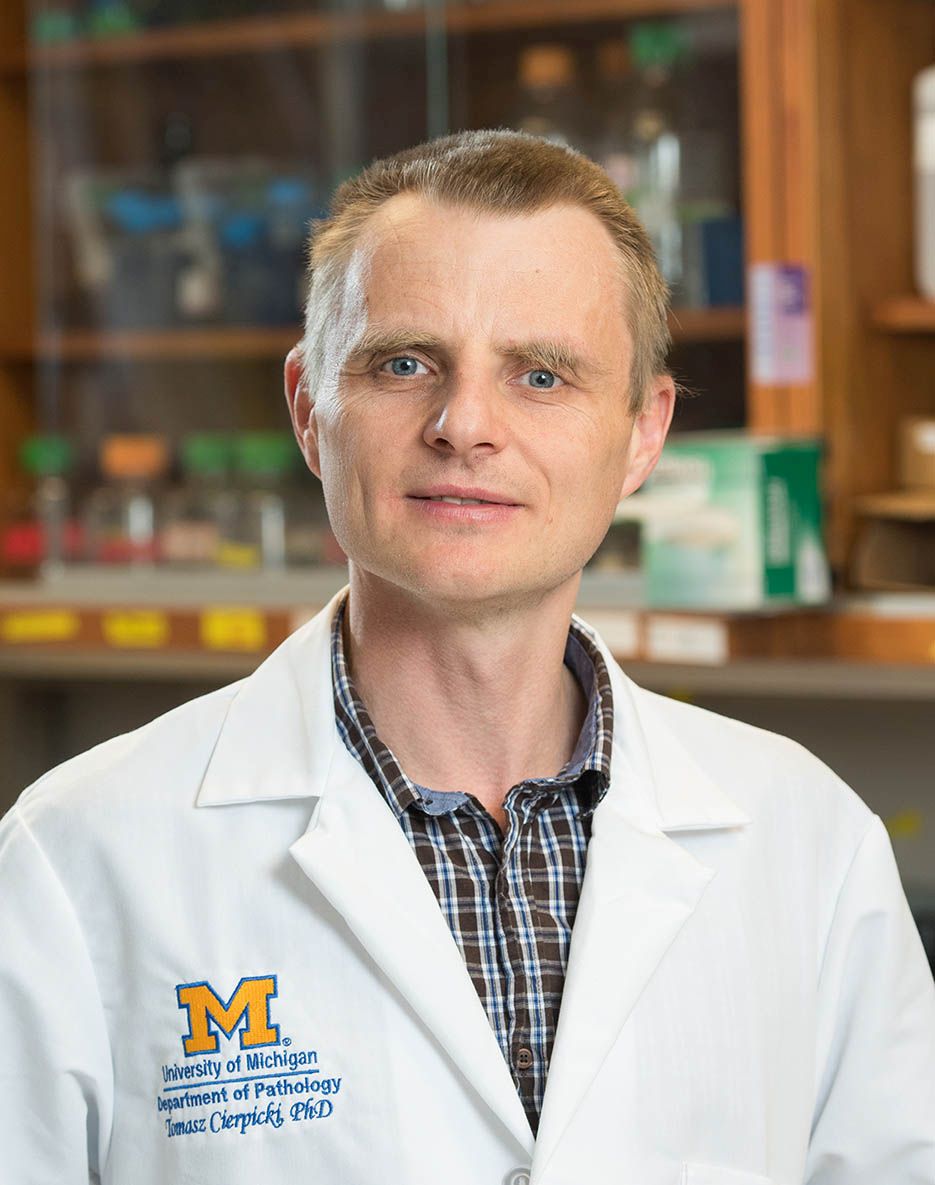
Tomasz Cierpick, Ph.D. Biography Publications
Jolanta Grembecka, Ph.D. Biography Publications
Venkateshwar Keshamouni, Ph.D. Biography Publications
2017 Forbes Scholars

Judy Leopold, Ph.D.
Drugging the Undruggable: Designing of Novel KRAS Inhibitors by Dual Targeting of the Effector and Allosteric Binding Sites.
Collaborative team of Dr. Judith Seboldt-Leopold (Departments of Radiology and Pharmacology) and Dr. Carol Fierke (Department of Biological Chemistry).
The KRAS oncogene is the most frequently mutated oncogene in human cancer. However, it has long been viewed as undruggable owing to the complexities associated with directly targeting this protein. The overall objective of our project is to design and optimize the development of small molecule inhibitors of KRAS protein-protein interactions to treat KRAS mutant cancers by simultaneously targeting the allosteric and effector binding pockets. Funding from the Forbes Institute will provide valuable assistance to enable the generation of proof of concept data to support our design approach.
Judy Seboldt-Leopold, Ph.D. Biography Publications
Carol Fierke, Ph.D. Biography Publications
James Moon, Ph.D.

Towards precision cancer immunotherapy
Collaborative team of Dr. James Moon (Departments of Pharmaceutical Sciences and Biomedical Engineering) and Dr. Evan Keller (Department of Urology)
Cancer immunotherapy has recently made a breakthrough with the clinical success of immune checkpoint inhibitors. However, despite their potential, immune checkpoint inhibitors benefit only a subset of patients. Therefore, there is a critical need for new strategies that can achieve potent and durable anti-tumor immune responses.
The team is working to address this major unmet clinical need by developing a new cancer vaccine technology that can work in synergy with immune checkpoint inhibitors. Dr. James Moon, in collaboration with Dr. Anna Schwendeman (assistant professors of Pharmaceutical Sciences), have produced ultrasmall (~10 nm in diameter) nanodiscs, composed of phospholipids and structural peptides. Preliminary studies performed in mice have shown that these nano-vaccines efficiently deliver tumor antigen peptides and adjuvants to lymphoid tissues and elicit striking levels of anti-tumor T-cell responses. When combined with immune checkpoint inhibitors, the vaccine nanodiscs eliminated tumors within 10 days of treatment in the majority of the mice. After waiting 70 days, researchers then injected the same mice with the same tumor cells, and the tumors were rejected by the immune system and did not grow, indicating that the animals developed immunity against tumor recurrence.
In this project supported by the Forbes Institute program, the researchers are now aiming to further develop the technology for personalized cancer vaccination. Because the majority of somatic mutations in cancer cells are unique to each patient, cancer vaccines would require a personalized approach. The team aims to harness the recent innovations in tumor exome sequencing to discover neo-antigens and develop a general strategy for personalized cancer vaccination using the nanodisc strategy.
James Moon, Ph.D. Biography Publications
Evan Keller, MPVM, DVM, Ph.D. Biography Publications
Nouri Neamati, Ph.D.
Discovery of next-generation therapeutics through machine learning techniques
Collaborative team of Dr. Nouri Neamati (Department of Medicinal Chemistry), Dr. Mats Ljungman (Department of Radiation Oncology), Dr. Vaibhav Sahai (Department of Internal Medicine, Hematology/Oncology), and Dr. Duxin Sun (Department of Pharmaceutical Sciences, College of Pharmacy)
To facilitate lead identification, the early and perhaps most critical step in drug discovery, we built a database of over 20 million small compounds that is searchable in two and three dimensions. Using machine learning techniques coupled with intensive bioinformatics analysis we can match pairs of compounds with similar mechanism of actions. The Forbes Institute grant will enable us to expand the use of this turnkey technology and to pursue the preclinical development of a very promising compound for the treatment of pancreatic cancer identified in our laboratory. To successfully complete this project, our team includes Dr. Neamati, an expert in drug design and discovery, Dr. Ljungman, who developed a novel next-generation sequencing technology, Dr. Duxin Sun, who has in-depth knowledge in PK/PD, and Dr. Vaibhav Sahai, a prominent medical oncologist with expertise in pancreatic cancer clinical trials.
Nouri Neamati, Ph.D. Biography Publications
Mats Ljungman, Ph.D. Biography Publications
Vaibhav Sahai, M.D. Biography Publications
Duxin Sun, Ph.D. Biography Publications
Lonnie Shea, Ph.D.

A synthetic pre-metastatic niche for early metastasis detection
Collaborative team of Dr. Lonnie Shea (Department of Biomedical Engineering) and Dr. Jacqueline S. Jeruss (Departments of Surgery, Pathology, and Biomedical Engineering)
The foundation of the proposed studies is that we (Jacqueline Jeruss and my laboratories) have developed an implant that captures early metastatic cells, and the combination of these implants for early detection combined with an early intervention can improve outcomes. Additionally, we have determined that the attraction of tumor cells to the implant results from the immune cells that are attracted to the implant.
The Forbes funding was based on a proposal to develop an early detection system based on the immune cells that are present in the implant, which differs in healthy relative to tumor bearing recipients. The detection of immune cells in the implant can potentially be used to identify the initiation of cancer prior to the spread of cells. While many investigators have proposed to sample the blood to look for cancer cells, our approach is unique in that the implant mimics a metastatic site and we are looking to determine whether the site is being prepared for the arrival of cancer cells, which occurs prior to the spread of disease. The properties we measure in the implant are not detectable in the blood.
The Forbes funded thus provides the seed to take the basic technology of the implant and develop a novel early diagnostic, which may ultimately enable a molecular staging of metastatic disease.
Lonnie Shea, Ph.D. Biography Publications
Jacqueline S. Jeruss, M.D., Ph.D. Biography Publications

Yu-Chih Chen, Ph.D., Emerging scholar
Yu-Chih Chen received his Ph.D. degree in Electrical & Computer Engineering at the University of Michigan, Ann Arbor in 2014, and he is currently a research faculty in both ECE and Cancer Center of the University of Michigan, Ann Arbor. Having both expertise in microfabrication and cell biology, he aims to develop the technology enabling cancer discovery. His current research focuses on microfluidic high-throughput single-cell analyses, focusing on the whole transcriptome sequencing of circulating tumor cells (CTC). Clinical CTC samples generally contain small number (~tens) of cells with a large amount of WBC's/RBC's contamination, yet analyzing them is essential for precision medicine. The small sample creates a challenge for microfluidic technology, which has shown enormous advantages over conventional assays. To overcome this challenge, the team has developed a highly sample efficient single-cell capture microfluidic architecture designed by flow circuit analysis and multi-layer microfabrication to achieve an unprecedented high cell capture efficiency (~65%). By combining the high-efficiency hydrodynamic cell capture scheme with a RNA barcoding technique, we enable single-cell whole transcriptome analysis (Hydro-Seq) for CTC samples. The single CTC cells can then be profiled using Next Generation Sequencing to understand the nature of disease. The technology we developed will ultimately provide better cancer treatment selection and prognosis monitoring for patients.
