Thyroid cancer genome analysis finds markers of aggressive tumors
Media contact: Nicole Fawcett, 734-764-2220 | Patients may contact Cancer AnswerLine™, 800-865-1125

TCGA study reveals molecular underpinnings; could lead to more precisely targeted treatment recommendations
ANN ARBOR, Mich. — A new comprehensive analysis of thyroid cancer from The Cancer Genome Atlas Research Network has identified markers of aggressive tumors, which could allow for better targeting of appropriate treatments to individual patients.
The finding suggests the potential to reclassify the disease based on genetic markers and moves thyroid cancer into a position to benefit more from precision medicine.
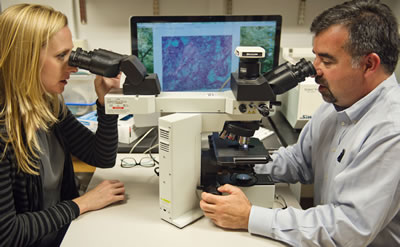
“This understanding of the genomic landscape of thyroid cancer will refine how it’s classified and improve molecular diagnosis. This will help us separate those patients who need aggressive treatment from those whose tumor is never likely to grow or spread,” says Thomas J. Giordano, M.D., Ph.D., professor of pathology at the University of Michigan Medical School.
Giordano is the project co-lead for TCGA thyroid cancer analysis along with Gad Getz, Ph.D., director of Cancer Genome Computational Analysis at the Broad Institute.
Thyroid cancer incidence has increased three-fold over the last 30 years and is the most rapidly increasing cancer in the United States. While the tumors are often slow-growing and easily treated with a combination of surgery, thyroid hormone and radioactive iodine, some patients will develop more aggressive and deadly thyroid cancers.
In this TCGA study, which is published in Cell, the researchers analyzed nearly 500 thyroid cancer samples to identify all genetic mutations that play a role. They found several new cancer genes as well as new variations of existing genes.
Overall, the thyroid cancer genome is relatively quiet, with fewer genetic mutations involved than in other common cancers, the researchers found. This may explain why the disease is often slow-growing.
Fewer mutations meant the researchers were able to look at the signaling pathways involved and understand what drives thyroid tumors. This approach helped them understand the genetic drivers of more of these cancers, reducing the percentage of “dark matter” cases – those with unknown genetic drivers – from 25 percent to 3.5 percent.
Those drivers can be broken down into two primary oncogenic groups: BRAF plus similar mutations and RAS plus similar mutations. But within these two primary groups, especially the BRAF group, several different subtypes of thyroid cancer exist. Currently, all thyroid cancers associated with BRAF, for example, had been considered essentially the same. That’s not the case.
“This study integrated a wide variety of genomic data to not only identify cancer drivers, but to compare how these different drivers behave,” said Getz, who is also director of the Bioinformatics Program at the Massachusetts General Hospital Cancer Center and an associate professor of pathology at Harvard Medical School. “Interestingly, we found that subsets of BRAF-mutated thyroid cancers are driving cancer through distinct mechanisms, and that some of these subsets are associated with higher risk and less differentiated cancers.”
The researchers used this understanding to create measures or scores that can determine how a tumor signals and how aggressive a thyroid tumor is. These scores are being tested in a clinical trial to assess if it can lead to more targeted treatment recommendations.
“These findings are a major step forward in how doctors and patients will address thyroid cancer diagnosis and treatment. Researchers around the world will be using this data, coming back to it and asking other scientific questions,” says Carolyn Hutter, Ph.D., M.S., program director in the division of genomic medicine at the National Human Genome Research Institute.
An initial recommendation is for the pathology and scientific communities to consider reclassifying thyroid cancer based on molecular subtypes to better reflect their underlying molecular properties. This would allow doctors to identify the slow-growing tumors from the aggressive tumors and recommend appropriate treatments.
The Cancer Genome Atlas is a federally funded project to understand the molecular characterization of various cancer types. The project has already published numerous signature papers in cancer types such as breast, colon, ovarian and lung. Thyroid cancer includes one of the largest sample sizes, with nearly 500 tumors studied.
Funding: National Institutes of Health grants 5U24CA143799, 5U24CA143835, U24CA143840, 5U24CA143843, 5U24CA143845, 5U24CA143848, 5U24CA143858, 5U24CA143866, 5U24CA143867, 5U24CA143882, 5U24CA143883, 5U24CA144025, U54HG003067, U54HG003079, U54HG003273 and P30CA16672
None
Reference: Cell, Vol. 159, No. 3, Oct. 24, 2014, DOI: 10.1016/j.cell.2014.09.050
