Pancreatic Survival Rates Improving
Media contact: Nicole Fawcett, 734-764-2220 | Patients may contact Cancer AnswerLine800-865-1125

More funding, scientific insights and clinical advances have started to drive progress in this challenging disease, and researchers see potential for immunotherapy to revolutionize its future.
When the five-year survival rate for pancreatic cancer hit 9 percent in 2017, it represented a near doubling from 5 percent just five years earlier.
While progress is exciting, researchers remain unsatisfied. So much work remains to be done.
“There’s actual reason for hope now. For the longest time, we were throwing around the word ‘hope,’ but now we have scientific reason for hope,” says Clifford Cho, M.D., a pancreatic cancer surgeon at the University of Michigan Rogel Cancer Center.
“I feel there’s momentum right now. Scientists are working tremendously hard on this question. There is an accelerating momentum. Our patients deserve that,” says Cho, C. Gardner Child Professor of Surgery and chief of hepatopancreatobiliary and advanced gastrointestinal surgery at Michigan Medicine.
Better funding throughout the last decade from foundations and advocacy organizations has helped move the field forward. Working collaboratively within and across institutions, researchers are gaining new understandings of the unusual biology of pancreatic cancer and can now simulate it better in laboratory models.
The result: incremental yet significant improvements in surgery, radiation therapy and chemotherapy that have some patients with advanced disease living for years instead of months.
And on the horizon: a determination among researchers to manipulate the immune system so that pancreatic cancer patients can benefit from the immunotherapy treatments revolutionizing other hard-to-treat cancers.
“Immune therapy is the future. For the past 20 years, we’ve been using chemotherapy regimens with minor benefits. We need more tolerable medicines that allow for a good quality of life,” says Howard Crawford, Ph.D., director of the Pancreas Disease Initiative and professor of molecular and integrative physiology and internal medicine at U-M.
“Pancreatic cancer has been one of the most difficult cancers, no question,” he says.
The statistics are bleak. About 55,440 people will be diagnosed with pancreatic cancer in 2018 and about 44,330 will die from the disease, according to the American Cancer Society.
And despite the incremental improvements in overall survival, a recent study predicted pancreatic cancer will become the second-leading cause of cancer-related death in the United States by 2020. It’s currently third.
Detecting pancreatic cancer in the early stages a challenge
The pancreas is an organ about the size of a hand that makes insulin and enzymes for digestion. It sits across the upper abdomen, behind the lower part of the stomach — more or less in the middle of your body.
And that makes it really hard to detect cancer.
Pancreatic cancer causes few symptoms and when they emerge, it’s often when the cancer is no longer curable through surgery.
“Early detection is important for pancreatic cancer. Patients come in with potentially precancerous lesions and within a year, it can progress from precancerous to metastatic,” says Vaibhav Sahai, MBBS, M.S., assistant professor of hematology and oncology at U-M.
“Patients don’t have symptoms early on and almost always present with advanced disease.”
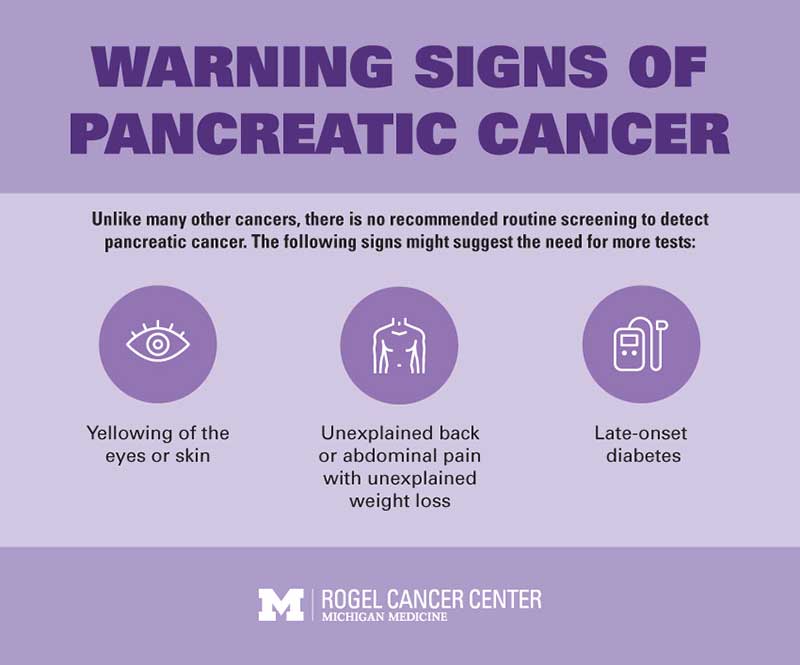
The most common symptoms -- unexplained back pain, unexplained weight loss, yellowing of the eyes or skin -- are general enough to blame on other problems. Many people are sent to a chiropractor when they first report unusual back pain.
“We need to do a better job of educating people and providers to be more alert when symptoms arise. Too many people are not having their symptoms recognized,” says Timothy Frankel, M.D., assistant professor of surgery at U-M.
There are no proven screening methods for pancreatic cancer and there aren't any specific risk factors
Currently, there are no proven effective screening tests for pancreatic cancer. Research is focused on using ultrasound or finding factors in the blood or urine that might serve as early markers.
Rogel Cancer Center researchers are working to detect circulating tumor cells or RNA markers of pancreatic cancer in the blood. Others are developing a scaffold device that could be inserted in the body to attract cancer cells, potentially triggering an early warning of a developing tumor.
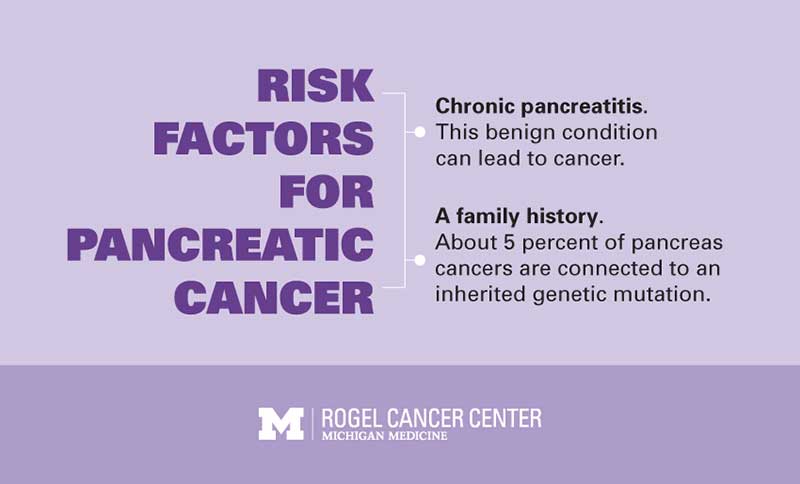
But the question is: Who should get these screenings? A small proportion of pancreatic cancers involve an inherited defect in genes such as BRCA1, BRCA2 or PALB2. This is likely around 5 percent of patients.
There are a few other indications that might suggest high risk, including other rare inherited gene defects, a first-degree relative with pancreatic cancer, and a new diagnosis of diabetes in middle-aged people without obesity. The only controllable risk factor is cigarette smoking..
Beyond these, little is known about why someone has a high risk of developing pancreatic cancer.
And then, if a screening test did exist, what would happen with someone at high risk or with a positive screening test?
“We need both better screening and better treatments. It’s not either/or,” says Marina Pasca di Magliano, Ph.D., associate professor of surgery and of cell and developmental biology at U-M. “Even if we have great screening tools, we will also need effective therapies.”
Why pancreatic cancer is so challenging
Several unique characteristics make pancreatic cancer especially difficult to treat.
It grows in an unusual pattern in which tentacles extend into the nerves and blood vessels. This creates challenges for surgeons and radiation oncologists who must work around these critical structures. It’s one reason only 20 percent of patients can have surgery.
It’s also very quick to metastasize. Too often, pancreatic cancer is diagnosed in late stages when it’s spread throughout the body. In animal models of precancerous lesions, researchers see cells being shed into the bloodstream -- signs that the cancer is metastasizing even before a tumor has formed.
“Even when we find it at the smallest size, sometimes it’s spread throughout the body,” Frankel says.
And even when patients can have surgery, this insidious cancer frequently returns. Only 1 in 4 patients survive long term after surgery.
Once the cancer spreads, it spreads everywhere. So when it reaches the liver, for example, it doesn’t usually form one tumor --— it forms dozens of tumors all throughout the organ, making it impossible to remove with surgery.
But improvements in imaging, surgical techniques and anesthesia mean more patients can benefit from surgery. Surgeons are using sophisticated imaging techniques to determine when cancer has advanced into nearby structures. Chemotherapy and radiation can shrink the tumor, unraveling it from critical structures or making it small enough that the patient can have surgery.
Pancreatic cancer cells are structured to protect them from chemotherapy
Surgery and radiation are often coupled with chemotherapy to kill any cancer remaining in the body. Recent improvements in chemotherapy, notably the drug combination FOLFIRINOX, have improved outcomes.
But another unusual hallmark of pancreatic cancer limits success.
“If you look at pancreatic cancer under a microscope, it doesn’t look like cancer. It looks like scar tissue with little spots of cancer,” Cho says.
This scar tissue, or fibrosis, increases pressure inside the tumor and causes blood vessels to collapse. When that happens, the chemotherapy drugs pumped through the veins don’t actually get into the tumor.
“If the tumor doesn’t see the chemotherapy, it doesn’t really do anything,” Crawford says. “All it does is make the patient sick.”
Research at the Rogel Cancer Center is looking at how to decrease fibrosis and diminish pressure on the blood vessels. Current clinical trials open at U-M are investigating approved drugs -- both novel and existing -- in new combinations to address this.
What’s tricky, though, is that this isn’t normal scar tissue. When researchers look at pancreatic cancer tissue samples, they see the tumor, the stroma and the rest of the tumor microenvironment composed of different types of cells.
“Typically, scar tissue is quiescent, but these are active and secreting a lot of signals. It’s similar to scar tissue but different,” Pasca di Magliano says. “People are starting to unravel what these cells do.”
Better research models bring big steps forward
Progress really began to open up in 2003 when researchers finally created a good mouse model of pancreatic cancer. Previous models struggled to express the correct cancer-driving genes or express them at the right level, so cancer in a mouse didn’t behave the same as cancer in a human.
Now, the pancreatic cancer mouse model is considered one of the closest to replicating human disease.
“We went from having no good model to having one of the best. The models have really led to the field exploding,” Pasca di Magliano says.
Researchers also began to improve upon traditional cell lines, which reflected only the tumor cells -- but not all of the other complicated systems at play in the stroma and microenvironment. Now, they can create three-dimensional organoids that better mimic what’s happening in the pancreas.
Another approach is to take tumors directly from patients and implant them into mice. These models can also capture key aspects of human pancreatic cancer for testing in the laboratory.
But because so few patients can have surgery, tissue samples are limited. The ultimate goal is to use tissue obtained from the biopsy that all patients undergo. Initial work in Pasca di Magliano’s lab suggests that the small amount of tissue obtained in a biopsy provides enough cells to grow into organoids.
The hope is to use individual patients’ tissue samples to create organoids, test multiple therapies and assess what’s most likely to be successful, based on genomic or epigenomic markers. Rogel Cancer Center researchers have been building up a biobank to understand this better.
KRAS mutations prove a tricky target
The most common genetic driver of pancreatic cancer comes from mutations in the KRAS gene, which account for 90 percent of pancreas tumors. This looked like the perfect target for treatment.
Instead, attempts to develop targeted therapies have failed. As of today, KRAS is considered undruggable.
“The driver mutation for this cancer has not been targetable. If you can’t target the driver, killing the passenger will not produce a cure,” Sahai says, explaining why current targeted therapies ultimately fail.
KRAS is like a small, tight ball. It leaves no surface or pocket where an inhibitor can notch its way in.
“Knowing we don’t have an agent to block KRAS, we are trying to understand what happens downstream,” Pasca di Magliano says. She’s working with Sahai to identify a combination of existing drugs that might be viable in a clinical trial.
The promise of immunotherapy
“If we are going to get to a cure or major advance for pancreatic cancer," Timothy Frankel, M.D. predicts, "it’s going to be through immunotherapy,"
What has researchers truly excited is immunotherapy. Harnessing the immune system to attack cancer has led to cures in advanced melanoma and lung cancer — cancers that previously had outcomes as bleak as pancreatic cancer.
So far, immunotherapy has been largely ineffective in pancreatic cancer. Still, researchers think they can solve it.
“The ability of the immune system to see pancreatic cancer is really zero,” Cho says. “But this is not insurmountable. Are there things we can do to pancreatic cancer to make it more noticeable to the immune system?”Our immune systems are wired to kill any foreign cells, including cancer cells. But cancer is wily. It finds ways to trick the immune system into thinking it belongs, essentially blocking the immune system from doing its job. The immunotherapy drugs that have worked in melanoma, immune checkpoint inhibitors, block this process.
But in pancreatic cancer, there are multiple mechanisms blocking the immune system.
“It’s been hard to get immune cells to go into the pancreas. We don’t see a lot of T cells, the killer immune cells,” says Ted Lawrence, M.D., Ph.D., Isadore Lampe Professor and chair of radiation oncology at U-M. “Immune checkpoint inhibitors won’t work if T cells aren’t getting there.”
He and collaborators Meredith Morgan, Ph.D., associate professor of radiation oncology, and Weiping Zou, M.D., Ph.D., Charles B. de Nancrede Professor of Surgery, Immunology and Biology, are working on an approach combining radiation with a new drug that affects DNA repair.
The idea: Trick the cell into thinking a virus is attacking. That then triggers the immune system, which would open the door for an immune checkpoint inhibitor to do its job. The approach has worked well in the lab, and plans for a clinical trial are underway.
Other groups at the Rogel Cancer Center are using techniques to analyze each individual cell to get a comprehensive view of what’s happening within the tumor. They hope this leads to an understanding of what signals are blocking the immune system and what vulnerable points to go after.
“Pancreatic cancer sets up an immunosuppressive shell that protects it from treatment,” Frankel says. “We’ve found ways to manipulate portions of the immune system, but this is one of the most immune-suppressed cancers. We think we can get around it and have had success in cell and animal models.
Exploiting how cells use energy
One potential vulnerability is in the metabolism, or the way cells use energy.
The body sends a limited amount of fuel to both the cancer and the immune system. The immune system needs fuel to kill the cancer. But the cancer gobbles up the nutrients, taking more than it needs. Immune cells, starved of nutrients, become exhausted, sluggishly sitting on the edges.

“Tumors find a dozen different ways to keep the immune cells away -- masking themselves, eating the nutrients,” says Costas Lyssiotis, Ph.D., assistant professor of molecular and integrative physiology at U-M. “If you can block how cancer cells are eating the nutrients, then immune cells can use those nutrients.”
His lab has pinpointed several unique metabolic differences specific to the pancreas, and is developing drugs to exploit them. Most of the testing is still in mice, but a phase 3 clinical trial will open soon at the Rogel Cancer Center comparing chemotherapy alone versus chemotherapy plus a metabolomic drug that switches off two pathways of energy.
Boom in clinical trials holds promise
It’s one of many for pancreatic cancer patients, demonstrating how progress in understanding the disease’s biology has led to novel ideas for combining drugs to improve outcomes.
“We now have a wide range of clinical trials for pretty much any stage of pancreatic cancer. This is how we learn what works or what doesn’t work,” Cho says.
Combine this with a new approach researchers are calling phase minus-1, including animal models and human three-dimensional organoid models running at the same time. This design keeps the pipeline flowing from the lab to the clinic and back -- a way to tweak and improve ideas as researchers gain more understanding of what works and what doesn’t.
Collaboration like this is key, researchers say -- a plan of attack that includes reaching out to scientists at other institutions to pool data and patient samples. Crawford and Pasca di Magliano are part of an NIH-funded consortium of researchers from six top cancer centers across the country.
The network will look at factors in the tumor microenvironment that make pancreatic cancer unresponsive to immunotherapy treatments and consider how to use already FDA-approved drugs to make pancreatic cancer responsive to immune therapy.
“The pancreatic cancer field in general is a very collaborative group. This is such a bad disease. It doesn’t matter who makes progress,” Crawford says. “Research funding for pancreatic cancer is very low, but beyond just money we need a smart approach to understanding this disease.”
Advocacy groups, such as the Pancreatic Cancer Action Network, are stepping forward to support this research, generating more funding and drawing top scientists to this difficult field. It’s starting to lead to advances and also helping to generate more collaboration.
Still, financial backing remains a crucial but finite resource.
“We have an unlimited amount of ideas. If you want to make something happen, there needs to be money in place,” Lyssiotis says. “We each have hundreds of ideas. I’m funded to try 10 of them. Did I pick the right 10? I picked the best 10, but this is science. If I had twice the funding, I could try twice as many ideas.”
Although finding a cure for pancreatic cancer seems like a lofty goal, researchers say “cure” is a loaded word.
Looking ahead, they’re encouraged by extended survival from incremental advances, and the promise of immunotherapy could lead to a giant leap forward.
“I think we’re going to get to the point very soon where we make pancreatic cancer as treatable as other cancers,” Crawford says. “Patients can have quality of life and longevity that allows them to live out a normal life with cancer as a chronic disease. That would be a huge difference.”
