Gene therapy for glioma improved survival in early research
Media contact: Anna Megdell, 734-764-2220 | Patients may contact Cancer AnswerLine™ 800-865-1125/p>
The first human trial combining drug therapy and immunotherapy for glioma patients shows promise
A study from the University of Michigan Department of Neurosurgery and Rogel Cancer Center shows promising early results that a therapy combining cell-killing and immune-stimulating drugs are safe and effective in extending survival for patients with gliomas, a highly aggressive form of brain cancer.
The study was published in The Lancet Oncology.
This is a phase 1, first in human trial, and Rogel researchers Pedro Lowenstein M.D., Ph.D., and Maria Castro, Ph.D., lead authors of the study, previously developed and studied the adenoviral mediated gene therapies in their lab.
Given gliomas’ poor prognosis and limited response to treatments like chemotherapy and radiation, the team looked to using the protein Flt3L to recruit immune cells, typically absent from the brain.
These immune cells are required to kick start a more effective cancer immune response.
“Being able to move a novel therapy from bench to bedside in such a streamlined fashion is exciting, and represents a tour-de-force in translational medicine,” said Oren Sagher, M.D., professor of neurosurgery at U-M and author of this study.
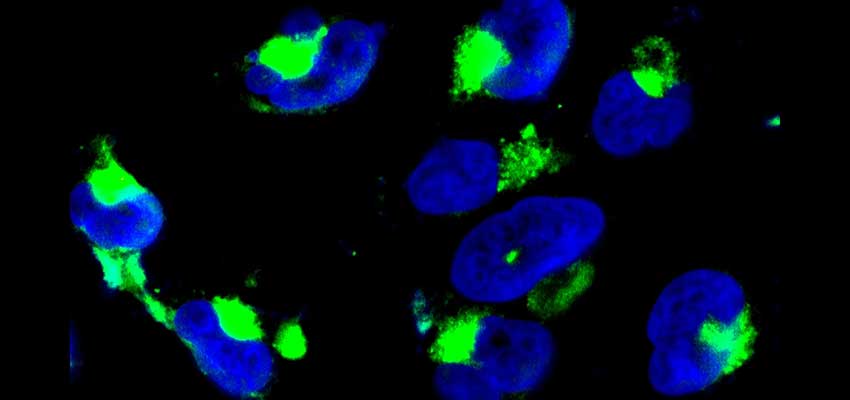
The study focused on two types of genetic therapies in high-grade gliomas.
The first was a combination of HSV-1-TK, a protein, and Valtrex, a drug used to treat viral infections like cold sores and chickenpox.
HSV-1-TK turns Valtrex into a cytotoxic compound that kills actively dividing cancer cells. The second was Flt3L, a protein that recruits essential immune cells to the brain.
When used in combination, these therapies showed exciting early results, including improved survival. Of the 18 patients enrolled in the trial, six survived more than two years, three survived more than three years, and one patient, who is still alive at the time of publication, survived up to five years.
With current standard-of-care, the life expectancy for a tumor of this kind of just over 14 months.
Further, the study found that this treatment wasn’t toxic to the patients, suggesting that the highest dose used in this trial could be used in future trials.
Though the adenoviral gene therapy vectors were supposed to be active for up to a month, work from three investigators—Maria Luisa Varela, Ph.D., Mohammad Faisal Syed, Ph.D., and Molly West, Ph.D.–discovered that activity from the adenoviral vector expressing the HSV1-TK was active for up to 17 months.
This discovery changes expectations of adenoviral gene therapy in the brain and extends the potential time during which the combination HSV1-TK and Valtrex might be harnessed to combat tumor recurrence.
“This originated from a theoretical idea based on evolutionary hypotheses and was first tested in experimental models of the disease,” said Lowenstein, Richard C. Schneider Collegiate Professor of Neurosurgery at U-M.
“Finally, after many years, we’re thrilled to report the results of testing this approach in human patients, obtaining results that will lead to better treatments for this group of brain tumor patients,” said Maria Castro, Ph.D., Rogel member and professor of neurosurgery at U-M.
Although more work is needed before this is brought to the clinic, the significance of long term expression of HSV1-TK suggest implementation to improve treatment.
The results of this study support the design of future phase 1b/2 clinical trials.
Additional authors include: Yoshie Umemura, M.D., Daniel Orringer, M.D., Larry Junck, M.D., Maria L. Varela, Ph.D., Molly E.J. West, M.S., Syed M. Faisal, Ph.D., Andrea Comba, Ph.D., Jason Heth, M.D., Oren Sagher, M.D., Denise Leung, M.D., Aaron Mammoser, M.D., Shawn Hervey-Jumper, M.D., Daniel Zamler, B.S., Viveka N. Yadav, Ph.D., Patrick Dunn, B.S., Wajd Al-Holou, M.D., Todd Hollon, M.D., Michelle M. Kim, M.D., Daniel R. Wahl, M.D., Ph.D., Sandra Camelo-Piragua, M.D, Andrew P. Lieberman, M.D., Ph.D., Sriram Venneti, M.D., Ph.D., Paul McKeever, M.D., Ph.D., Theodore Lawrence, M.D., Ph.D., Ryo Kurokawa, M.D., Ph.D., Karen Sagher, B.S., David Altshuler, M.D., Lili Zhao, Ph.D., Karin Muraszko, M.D.
Funding: Phase One Foundation, Los Angeles, CA, The Board of Governors at Cedars-Sinai Medical Center, Los Angeles, CA, and The Rogel Cancer Center at The University of Michigan; clinicaltrials.gov: NCT01811992
Paper cited: “A non-randomized, open-label, dose-finding, first-in-human trial of combined cytotoxic and immune-stimulatory gene therapy for primary adult high-grade glioma,” The Lancet Oncology. DOI: 10.1016/S1470-2045(23)00347-9
